
Single-port laparoscopic and transvaginal resection of a large pelvic aggressive angiomyxoma: a case report
Introduction
Aggressive angiomyxomas (AAM) are rare mesenchymal neoplasms that tend to grow in the pelvis and perianal regions (1-9). They occur more frequently in premenopausal than postmenopausal women, with a peak incidence in the forties (2,3). These tumours are considered aggressive due to their infiltrative nature, with reports of invasion to areas such as the vulva and perineum (3). However, metastasis to other distant sites in the body is rare, and the general prognosis is good (4). The mainstay of treatment is surgical excision, aiming to achieve optimal debulking, which has been performed via various approaches, such as a transperineal or pararectal incision, minimally invasive technique, or laparotomy (5-10). For oncological surgeries, access to the tumour without excessive handling and resection of the mass with clear margins is essential to avoid adverse outcomes. The benefit of laparotomy is the exposure of the neoplasm. However, it is associated with morbidities such as more pain, a longer hospitalisation stay and slower recovery. For a laparoscopic approach, the benefits include less pain and faster recovery. As AAMs are often soft to a firm consistency, there is a risk of rupture of the tumour during handling or retrieval. By performing via a transperineal or pararectal approach, this can be beneficial in women with no concurrent gynaecological pathology or in patients who are Virgo intacta. If the tumour extends proximally, it may be difficult to access the tumour, which may necessitate conversion to laparotomy.
We report the first case of single-port laparoscopic and transvaginal resection of a pelvic AAM to highlight the benefits of this novel approach. With single-port laparoscopy, the surgeon dissects the tumour under laparoscopic guidance and controls the tumours handling, hence avoiding excessive manipulation by assistants. Atraumatic instruments were used during dissection to avoid disrupting the tumour. Combining it with a transvaginal approach allows the retrieval of large specimens compared to laparoscopic incisions as the vagina is more spacious and avoids additional incisions over the perineum or abdomen. We present the following case in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-21-92/rc).
Case presentation
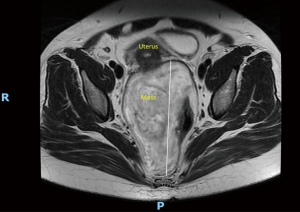
Our patient was a 45-year-old woman with two previous normal vaginal deliveries who presented with a vaginal lump of one year’s duration. The lump worsened over the past year, affecting her work and quality of life. She had issues with sexual intercourse but denied any obstructive urinary or bowel symptoms. She also complained of menorrhagia but no dysmenorrhea, intermenstrual bleeding, or post-coital bleeding. Her cervical cancer screening was up-to-date and normal. She had no past medical or surgical history and no family history of cancer. On examination, her vitals were stable. She was alert and well. The abdomen was soft and not distended with no palpable masses. A 20 centimetre (cm) soft mass was seen prolapsing from the posterior vaginal wall (Figure 1). A speculum examination could not clearly visualise the cervix as it was displaced anteriorly by the mass. A vaginal examination revealed a normal cervix and the vagina mucosa was smooth. The rectal mucosa was smooth on digital rectal examination and the mass was palpable anterior to the rectum. Subsequently, an ultrasound scan of the pelvis showed a 14.4 cm × 10.2 cm × 10.0 cm heterogeneous structure with vascularity, posterior to the uterus (Figure 2). The uterus was adenomyotic and the endometrial lining was four millimetres (mm). Both ovaries were normal. We ordered a magnetic resonance imaging (MRI) scan of the pelvis to further characterise the mass. On the MRI scan, there was a 23.9 cm × 12.7 cm × 8.4 cm extraperitoneal, mildly enhancing soft tissue mass sited between the uterus, vagina anteriorly and the rectum posteriorly, with preservation of the rectovaginal fascia (Figures 3,4). The mass had a significant prolapsed component through the perineum but showed no overt infiltration or invasion into the adjacent structures or sacrococcygeal spine. It was a T2W hyperintense and T1W hypointense mass with no significant restricted diffusion. The external anal sphincter was intact and there were no enlarged abdominal or pelvic lymph nodes. Given the examination and radiological findings, the differential diagnoses were angiomyxoma, leiomyoma with cystic degeneration, leiomyosarcoma or lipoma. As there was no signs of local invasion or distant metastasis, her prognosis was good.


Blood investigations done showed an iron deficiency anaemia with a haemoglobin level of 6.4 g/dL, but her creatinine level was normal. She was transfused with 2 pints of packed red blood cells and her haemoglobin increased to 9.3 g/dL pre-operatively. Due to her large retroperitoneal mass, she was counselled for surgical resection for diagnostic and therapeutic indications. A biopsy may not be representative of the tumour and may be inconclusive or inaccurate. As the woman had completed her family, she was keen for a total hysterectomy in the same setting for definitive treatment of her menorrhagia. Hence, she consented to diagnostic laparoscopy, total hysterectomy, bilateral salpingectomies and resection of the retroperitoneal mass for curative intent.
Surgical technique
We decided on a single-port laparoscopic approach, also known as laparoendoscopic single-site (LESS) surgery, for faster recovery, less postoperative pain, better cosmesis, and shorter hospitalisation stay (Video 1). We decided on this approach based on our clinical assessment and review of the radiological findings.
Pre-operatively, we performed a pelvic examination. As the woman was a multiparous lady, the vagina was capacious. We also reviewed the scan images to determine the consistency of the mass and its anatomy and relation to the surrounding structures. As most of the lump had prolapsed through the perineum, a transvaginal approach would be suitable and allow easy access and retrieval of the specimen. Moreover, the patient required a total hysterectomy for her concurrent gynaecological pathology, which could be performed transvaginally. Single-port laparoscopy would allow dissection of the tumour under direct vision.
Under general anaesthesia, she was placed in a lithotomy position. After cleaning and draping, we used a 5-mm optical trocar with the laparoscope to enter the abdominal cavity at the umbilicus under direct vision. The abdomen was insufflated with carbon dioxide gas to create a pneumoperitoneum. The 5 mm umbilical incision was extended to 2 cm. Subsequently, an extra extra small (XXS) Alexis® (Applied Medical Resource Corp, USA) retractor was inserted into the peritoneal cavity. We used a hand-made gloved port to attach to the Alexis® retractor. The gloved port consisted of a sterile size 7 1/2 left-hand glove. Three 5-mm ports and one 12-mm port were fitted into the thumb, index finger, middle finger and little finger sleeves and secured with sutures to prevent air leaks. For the rest of the surgical steps, we used a 30-degree rigid laparoscope, laparoscopic instruments, and energy device, i.e., LigaSure™.
Intra-operatively, the uterus was 12 weeks in size. There was a large retroperitoneal mass on the right side, of which 40 cm had prolapsed through the vagina. The mass extended to the right common iliac vessels and to the Pouch of Douglas. It was adherent to the pelvic sidewall, ureters and retroperitoneal space, and there was no direct involvement of the uterus, bowels, or ureters.
First, we dissected the broad ligament to open up the pelvic spaces. We traced and lateralised the right ureter. We then mobilised the sigmoid colon, dissected the peritoneum overlying the mass and the mass from the upper vagina. We proceeded to perform the hysterectomy and salpingectomies before doing a colpotomy. The uterus, cervix and both tubes were retrieved vaginally. The upper part of the mass, which was the largest diameter at 12 cm, was delivered through the vaginal vault. As the mass was soft, we could negotiate it through the vagina without requiring an extension of the incision as the vagina was stretchable and capacious. Furthermore, the mass was adherent to the rectum but not the anus and anal sphincters. Hence, we could deliver the lump through the vagina. The rectum was dissected away from the mass using diathermy. No incisions or dissection were required over the posterior part of the vagina wall. The vault was then closed transvaginally with absorbable braided sutures. This demonstrated that the rectum could be delivered through the vagina and the dissection of the rectum from the mass could be done under direct vision. An alternative approach would be to make an incision on the posterior vaginal wall, but in our opinion, this could increase the risk of injury to the rectum or anal sphincters.
Outcome
She underwent a single-port laparoscopic total hysterectomy, bilateral salpingectomies, and transvaginal resection of the retroperitoneal mass. Figure 5 showed the postoperative finding and Figures 6,7 were photos of the specimen. The estimated blood loss was 200 millilitres (mL). She was started on feeds on postoperative day one and escalated to diet on postoperative day two. The patient recovered well postoperatively and was fit for home on postoperative day two. The histology of the mass was consistent with an AAM. Histologic sections of the mass showed a fairly homogeneous appearance where the stromal cells were widely separated, bland with ovoid to spindle nuclei and had scanty cytoplasms. Immunohistochemistry performed showed that the cells stained strongly positive for oestrogen receptors (ER), progesterone receptors (PR), vimentin, desmin and patchy positivity for smooth muscle actin (SMA) and CD34. The uterus was adenomyotic with a benign endometrial polyp and the cervix and both tubes were normal. As of two and a half years’ follow-up, the patient did not have any recurrence. She had regained her quality of life and was well. There were no issues with prolapse or sexual intercourse.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Angiomyxomas tend to present as slow-growing tumours that may only be diagnosed incidentally or after years when the masses become clinically obvious to patients (2,11). Depending on the location of the mass, it can be challenging to diagnose it. Among the imaging modalities, an MRI scan is the best imaging technique to characterise the mass and aids in surgical planning by determining the extent of its growth. The typical appearance of AAM on MRI scans on T1-weighted images may be that of a “swirled” or “whorled” appearance with low or equal signal and high signal on T2-weighted images (1,3).
Surgical resection of angiomyxomas has been the main treatment modality with the aim of obtaining negative margins to reduce the risk of local recurrences (4,11). This may require extensive debulking surgery if the mass is large or infiltrates into surrounding structures such as the rectum or vagina, increasing surgical morbidity. The rate of local recurrence has been reported to range from 25% to 47% and is mainly thought to be due to inadequate excision (4,13,14). Alternative treatment options include hormonal therapy due to the high prevalence of ER and PR positivity among AAMs (1-4,8-12). The use of gonadotrophin-releasing hormone (GnRH) agonist or aromatase inhibitors have been reported to reduce the size of the tumours before surgery or as adjuvant therapy to reduce recurrence risk (2,15-17). However, these studies are generally retrospective with a small number of cases. Hence, prospective studies should be conducted to review the long-term outcomes of patients on hormonal treatment and the risk of recurrence on these treatments.
As we are a tertiary hospital in Singapore with expertise in LESS surgery, we chose this approach for this patient. The decision for this approach depended on the expertise and experience of the surgeon. The primary surgeon in this case was a gynaecology oncologist with expertise in performing MIS, especially LESS or robotic cases for oncological cases. Hence, we felt that this technique would be beneficial for patients without compromising overall outcomes. Single-port laparoscopy has been associated with low pain scores, short hospitalisation stay, faster recovery and better cosmesis than conventional laparoscopy (18). The use of a hand-made gloved port has been shown to be a feasible, low-cost, and easily reducible method for LESS surgeries (19).
To our knowledge, this is the first published report of using a single-port laparoscopic technique for surgical resection of a pelvic AAM. The benefit of this procedure allowed enucleation and complete resection of the AAM while preserving bladder and bowel functions. In addition, the transvaginal route allows dissection of the vagina from the retroperitoneal mass, easy retrieval of the specimen, avoiding external skin scarring and is less painful than extending the abdominal incision for specimen retrieval. We highlighted this novel approach that could be possible for patients with pelvis AAM. This approach can be useful in women undergoing hysterectomy in the same setting since the mass and rectum can be delivered through the vagina vault. The dissection of the mass from the rectum is also performed under direct vision, hence reducing the risk of injuries.
Kanao et al. (9) has demonstrated a combined laparoscopic and perineal approach to excise AAM. In their case, the mass extended down to the vulva and an incision on the vulva was required. In our case, as the mass had prolapsed through the vagina, we were able to excise it through the vaginal vault. This is an alternative approach for angiomyxomas that prolapse through the vagina.
More research needs to be done to study the long-term prognosis and add to the growing evidence on the role of MIS in the management of such patients. We acknowledge that we need longer follow-up to assess the long-term prognosis for our patient. However, it would be difficult to perform randomised controlled trials to compare the various surgical approaches due to this tumor’s rarity.
Conclusions
Minimally invasive approach is increasingly used in various oncological surgeries, especially gynaecology oncological cases. Our case demonstrates that a combination of single-port laparoscopic and transvaginal techniques can be performed with the benefits of complete enucleation and resection of the tumour, less scarring and lesser postoperative pain. This study provides a possible alternative surgical procedure for patients with AAM that experienced surgeons can perform safely.
Acknowledgments
The authors would like to acknowledge Mr. Ho Yin Shan for his narration of the video.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-21-92/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-21-92/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Amante S, Sousa R, Amaral R. Pelvic Soft Tissue Aggressive Angiomyxoma. J Belg Soc Radiol 2020;104:55. [Crossref] [PubMed]
- Hajjar R, Alharthi M, Richard C, et al. Pelvic Aggressive Angiomyxoma: Major Challenges in Diagnosis and Treatment. Cureus 2019;11:e4419. [Crossref] [PubMed]
- Fetsch JF, Laskin WB, Lefkowitz M, et al. Aggressive angiomyxoma: a clinicopathologic study of 29 female patients. Cancer 1996;78:79-90. [Crossref] [PubMed]
- Sutton BJ, Laudadio J. Aggressive angiomyxoma. Arch Pathol Lab Med 2012;136:217-21. [Crossref] [PubMed]
- Choi H, Park C, Ji YI. Alternative surgical approaches for aggressive angiomyxoma at different sites in the pelvic cavity. Obstet Gynecol Sci 2015;58:525-9. [Crossref] [PubMed]
- Iyibozkurt AC, Yasa C, Schmieta DE, et al. Aggressive angiomyxoma of the pelviperineum: surgical treatment through a perineal incision. J Minim Invasive Gynecol 2011;18:541-4. [Crossref] [PubMed]
- Dalvi AN, Garale MN, Churiwala JJ, et al. Pararectal angiomyxoma: a diagnostic dilemma. J Surg Case Rep 2019;2019:rjz331. [Crossref] [PubMed]
- Akhavan S, Nikfar S, Behboudi B, et al. Aggressive angiomyxoma of the pelvis surgical management in a case with delayed diagnosis. Int J Surg Case Rep 2021;81:105756. [Crossref] [PubMed]
- Kanao H, Aoki Y, Tanigawa T, et al. En Bloc Resection of an Aggressive Angiomyxoma by a Novel Combination Laparoscopic and Open Perineal Approach. J Minim Invasive Gynecol 2019;26:598-9. [Crossref] [PubMed]
- Aguilar-Frasco J, Ruben-Castillo C, Rodríguez-Quintero JH, et al. Aggressive angiomyxoma: giant recurrence successfully treated with wide excision and adjuvant therapy with GnRH analogue. BMJ Case Rep 2018;11:226973. [Crossref] [PubMed]
- Chen H, Zhao H, Xie Y, et al. Clinicopathological features and differential diagnosis of aggressive angiomyxoma of the female pelvis: 5 case reports and literature review. Medicine (Baltimore) 2017;96:e6820. [Crossref] [PubMed]
- Yalinkaya A, Askar I, Bayhan G, et al. Aggressive angiomyxoma of the female pelvis and the labium. Acta Obstet Gynecol Scand 2003;82:298-301. [Crossref] [PubMed]
- Kiran G, Yancar S, Sayar H, et al. Late recurrence of aggressive angiomyxoma of the vulva. J Low Genit Tract Dis 2013;17:85-7. [Crossref] [PubMed]
- Wang Q, Zhao M, Lin X, et al. Aggressive angiomyxoma of the vulva: intra-operative pathological diagnosis is useful in deciding the scope of surgery and reducing recurrence. Acta Chir Belg 2012;112:79-84. [Crossref] [PubMed]
- Fine BA, Munoz AK, Litz CE, et al. Primary medical management of recurrent aggressive angiomyxoma of the vulva with a gonadotropin-releasing hormone agonist. Gynecol Oncol 2001;81:120-2. [Crossref] [PubMed]
- Fucà G, Hindi N, Ray-Coquard I, et al. Treatment Outcomes and Sensitivity to Hormone Therapy of Aggressive Angiomyxoma: A Multicenter, International, Retrospective Study. Oncologist 2019;24:e536-41. [Crossref] [PubMed]
- Walczak K, Luczynska K, Kupryjanczyk J, et al. Long-term response to hormone therapy in a young woman with aggressive pelvic angiomyxoma. Ginekol Pol 2021;92:82-3. [Crossref] [PubMed]
- Tsai AY, Selzer DJ. Single-port laparoscopic surgery. Adv Surg 2010;44:1-27. [Crossref] [PubMed]
- Livraghi L, Berselli M, Bianchi V, et al. Glove technique in single-port access laparoscopic surgery: results of an initial experience. Minim Invasive Surg 2012;2012:415430. [Crossref] [PubMed]
Cite this article as: Ng QJ, Wu Y, Nadarajah R. Single-port laparoscopic and transvaginal resection of a large pelvic aggressive angiomyxoma: a case report. AME Surg J 2022;2:40.





