
Laparoscopic cholecystectomy in a patient with situs inversus totalis: report of a case with surgical tips
Introduction
Laparoscopic cholecystectomy (LC) is currently the gold standard therapy for cholelithiasis. Situs inversus totalis (SIT) is a rare congenital anomaly characterized by a mirror-image transposition of organs (1). Although SIT is rare (2), owing to the high prevalence of cholelithiasis, surgeons are likely to encounter patients with SIT in whom cholecystectomy is indicated. To date, approximately 100 cases of LC in patients with SIT have been reported in the English literature (3), and many of these studies have described that this approach is technically challenging owing to anatomical unfamiliarity in these patients. We report successful LC in a patient with SIT. We have additionally described practical tips for the LC procedure in patients with SIT, which would be useful to surgeons in routine practice. We present the following case in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-21-106/rc).
Case presentation
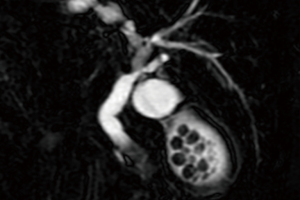
A 69-year-old female with no relevant medical history visited a local physician with a chief complaint of upper abdominal pain. Blood tests results showed abnormally high levels of hepatobiliary enzymes as follows: total bilirubin 1.5 mg/dL, aspartate aminotransferase 881 IU/L, alanine aminotransferase 509 IU/L, and gamma-glutamyl transpeptidase 190 IU/L; therefore, she was referred to our hospital on the next day for further evaluation. At the time of her visit to our hospital, abdominal pain had disappeared already. Computed tomography at our hospital revealed that all the visceral organs were located in the opposite side to the normal position, without any findings to suggest possible contributors to liver dysfunction (Figure 1). Blood tests revealed a reduction in hepatobiliary enzyme levels as follows: total bilirubin 0.9 mg/dL, aspartate aminotransferase 129 IU/L, alanine aminotransferase 273 IU/L, and gamma-glutamyl transpeptidase 126 IU/L. Magnetic resonance cholangiopancreatography performed a few days later revealed numerous gallbladder stones, without any evidence of stones in the common bile duct (Figure 2). Based on these findings, we concluded that a common bile duct stone was temporarily incarcerated in the duodenal papilla and was spontaneously excreted subsequently. Therefore, LC was performed to avoid recurrences.

Surgical techniques
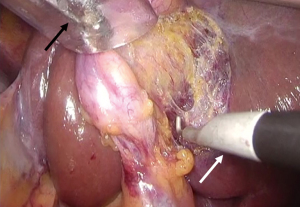
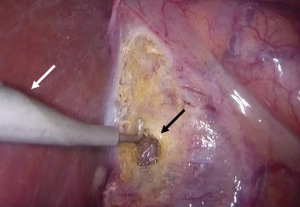
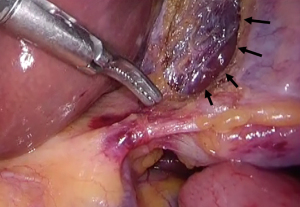
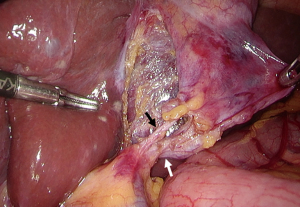
The surgical equipment was arranged on the side opposite to that used for routine LC (Figure 3). The patient was placed in the open-leg position, and the surgeon stood to the patient’s right, with the assistant to the left, and the camera assistant between the patient’s legs. A 12 mm trocar was inserted into the peritoneal cavity through the umbilicus using the open method, and pneumoperitoneum was created. Another 12 mm trocar was placed immediately inferior to the xiphoid process of the sternum, for insertion of instruments from the surgeon’s left. Two more subcostal 5 mm trocars were placed in the midclavicular and the left anterior axillary lines for manipulation of instruments by the surgeon’s right hand and for the assistant, respectively. Intraoperatively, we confirmed SIT; however, the gallbladder appeared nearly normal. Using a hook electrocautery, the surgeon made a serosal incision at the level of the infundibulum-cystic junction, and the incision was extended along both aspects of the gallbladder. Subsequently, using his left hand, the surgeon flipped the Hartmann’s pouch to the ventral aspect on the right, and using his right hand, performed dissection posterior to the gallbladder body to neck from the left side of the gallbladder (the side opposite to Calot’s triangle) (Figure 4). After dissection to the maximum extent possible on the posterior aspect of the gallbladder, using his right hand, the surgeon flipped the Hartmann’s pouch to the left. Using his left hand, the surgeon made a small incision posterior to the gallbladder body, which was immediately communicated with the dissected space from the left aspect (Figure 5). After creating adequate space posterior to the gallbladder neck to body (Figure 6), the surgeon cut the connective tissues around the cystic artery and the cystic duct and could successfully achieve the critical view of safety (CVS) (Figure 7). The cystic artery and the cystic duct were clipped and cut sequentially, and the gallbladder was detached from the liver and removed through the umbilicus. The operative time was 84 min with negligible bleeding. The patient’s postoperative course was uneventful.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
SIT is a rare autosomal recessive congenital anomaly characterized by the mirror-image transposition of visceral organs (4). The incidence of SIT ranges from approximately 1 in 8,000 to 1 in 25,000 of the general population (2). Notably, the incidence of cholelithiasis in patients with SIT is reported to be as high as that in the general population (non-SIT individuals) (5); therefore, surgeons should be familiar with such clinical presentations.
SIT is also known to be associated with various visceral malformations such as congenital heart disease, splenic malformation, intestinal malrotation, biliary atresia, and vascular anomalies (6). Vascular anomalies of the celiac trunk and liver are common in SIT patients (7), but it is unclear if anomalies of the cystic artery are frequent because there are few case reports. Only two cases of “inferior cystic artery” and “posterior cystic artery” have been reported as morphological abnormalities of the cystic artery in SIT patients (6,8). However, surgeons should be careful about such anomalies to avoid unexpected hemorrhage during cholecystectomy. In our case, we performed contrast-enhanced CT before surgery and confirmed that the cystic artery was located the mirror image of the normal position (Figure 1).
LC is currently the gold standard therapy for cholelithiasis. In 1991, Campos and Sipes (9) reported the first case of LC in a patient with SIT, and several studies have described similar cases since then. In a study that included 92 cases of LC performed in patients with SIT, Alkhlaiwy et al. (3) observed no severe complications and no conversion to open cholecystectomy in the study population, which suggests that the safety profile of LC in patients with SIT is comparable with that of LC performed in the general population. However, several studies have reported that LC in cases of SIT is technically challenging owing to the mirror-image anatomy of visceral organs. In view of the reversal of the anatomical positions of organs, the easiest solution is to reverse positioning of the surgical team and port sites. In fact, most authors prefer this method (3,10), which we too followed in this study. However, in such situation, dissection of Calot’s triangle using the right hand and simultaneous stretching of the Hartmann’s pouch using the left hand results in an awkward crossing of hands, which is inconvenient and demanding for surgeons (10,11). Several technical modifications have been reported to overcome this difficulty. A few studies have suggested that surgeons can use their left hand for dissection via the subxiphoid port during LC in cases of SIT (9,12). An alternative is the single-hand method during which the surgeon uses his right hand for dissection via the subxiphoid port, and the assistant stretches the Hartmann’s pouch and fundus of the gallbladder using both hands (10). However, we did not adopt these methods because meticulous dissection was not so easy using a non-dominant hand or a single hand.
Single incision laparoscopic cholecystectomy (SILC) seems to be another option. However, SILC in SIT has rarely been reported. Jhobta et al. (5) reported a case of SILC in SIT and described that the advantage of SILC is to be able to dissect by the surgeon’s right hand in addition to better cosmesis and reduced invasiveness. In our case, we did not select this method because we were not accustomed to SILC itself, but it may be easier than conventional LC for surgeons who are familiar to this method.
Even in routine LC, there are various methods depending on the institution or the surgeon as to which part of the gallbladder to start dissection. In our opinion, tunneling posterior to the gallbladder body before reaching the Calot’s triangle is an important step during LC to achieve CVS easily and safely, and we recommend this approach as a useful strategy even in cases of SIT. Using the right hand under double hand coordination, the surgeon can easily perform dissection on the posterior aspect of the gallbladder body from the left side (the opposite side to Calot’s triangle) (Figure 4); on the other hand, we observed that dissection on the right side of the gallbladder (the side of Calot’s triangle) using the surgeon’s right hand was technically challenging primarily because of awkward crossing of the surgeon’s hands and also because the direction to dissect and the direction of the right hand were perpendicular. However, in patients in whom dissection performed from the left aspect is sufficient, surgeons can easily perform tunneling posterior to the gallbladder neck from its right aspect even using their left hand (Figure 5). Having created sufficient space posterior to the gallbladder body to neck (Figure 6), CVS can be easily and safely achieved even in patients with SIT (Figure 7).
In conclusion, although SIT is rare, owing to the fact that prevalence of cholelithiasis in patient with SIT is comparable with that in the general population, surgeons should prepare for LC in patients with SIT. Intraoperatively, it is important to perform the dissection procedure from the left side of the gallbladder and ensure the creation of sufficient space posterior to the gallbladder body to neck before touching Calot’s triangle, for successful LC in patients with this rare congenital anomaly.
Acknowledgments
We would like to thank Editage (https://www.editage.jp) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-21-106/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-21-106/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-21-106/coif). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosen H, Petrosyan M, Mason RJ. Cholecystitis in Situs Inversus Totalis. Radiol Case Rep 2008;3:226. [Crossref] [PubMed]
- Lee SE, Kim HY, Jung SE, et al. Situs anomalies and gastrointestinal abnormalities. J Pediatr Surg 2006;41:1237-42. [Crossref] [PubMed]
- AlKhlaiwy O, AlMuhsin AM, Zakarneh E, et al. Laparoscopic cholecystectomy in situs inversus totalis: Case report with review of techniques. Int J Surg Case Rep 2019;59:208-12. [Crossref] [PubMed]
- Ren JJ, Li SD, Geng YJ, et al. Modified laparoscopic cholecystectomy technique for treatment of situs inversus totalis: A case report. J Int Med Res 2017;45:1261-7. [Crossref] [PubMed]
- Jhobta RS, Gupta A, Negi B, et al. Single-incision laparoscopic cholecystectomy using conventional instruments in situs inversus totalis. BMJ Case Rep 2018;11:e226404. [Crossref] [PubMed]
- Pavlidis TE, Psarras K, Triantafyllou A, et al. Laparoscopic cholecystectomy for severe acute cholecystitis in a patient with situs inversus totalis and posterior cystic artery. Diagn Ther Endosc 2008;2008:465272. [Crossref] [PubMed]
- Kulesza RJ Jr, Kalmey JK, Dudas B, et al. Vascular anomalies in a case of situs inversus. Folia Morphol (Warsz) 2007;66:69-73. [Crossref] [PubMed]
- Kamitani S, Tsutamoto Y, Hanasawa K, et al. Laparoscopic cholecystectomy in situs inversus totalis with "inferior" cystic artery: a case report. World J Gastroenterol 2005;11:5232-4. [Crossref] [PubMed]
- Campos L, Sipes E. Laparoscopic cholecystectomy in a 39-year-old female with situs inversus. J Laparoendosc Surg 1991;1:123-6.
- Arya SV, Das A, Singh S, et al. Technical difficulties and its remedies in laparoscopic cholecystectomy in situs inversus totalis: A rare case report. Int J Surg Case Rep 2013;4:727-30. [Crossref] [PubMed]
- Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech A 2001;11:233-7.
- Eisenberg D. Cholecystectomy in situs inversus totalis: a laparoscopic approach. Int Med Case Rep J 2009;2:27-9.
Cite this article as: Matsumoto T, Okawa T, Asakura Y, Sakamoto H, Arimoto A, Yokoyama K, Ueno N, Yoshikawa T. Laparoscopic cholecystectomy in a patient with situs inversus totalis: report of a case with surgical tips. AME Surg J 2023;3:10.



