
Reconstructive options of the chest wall after trauma: a narrative review
Introduction
Background
Despite the development of many methods for safety in the workplace, home and on roads, chest trauma retains a 60% rate in polytrauma with a mortality of about 20–25% (1,2). Moreover, chest trauma accounts for 15% of injuries affecting the emergency room and luckily only 10% of the total, requires a surgical approach (3). The patient’s general conditions should be stabilized early using orotracheal intubation and mechanical ventilation if necessary, associated with pain control and systematic toilet of airway. Although it is possible to achieve medium-/long-term recovery of respiratory function (4), prolonged conservative treatment exposes the patient to the risk of pneumonia, fibrosis and chest deformity as well as the inability to wean from ventilator (5).
Rationale and knowledge gap
If on the one hand there is unanimous consensus in the surgical approach of the flail chest, on the other hand there are doubts about fixation of isolated chest fractures (ICF). Untreated displaced ICF not only increase the risk of pneumothorax, hemothorax and pulmonary hernias (6) but can lead to chronic disunion/disruption of the stumps up to pseudarthrosis (7,8) with pain, reduced respiratory dynamics and dyspnea. A further point of discussion is the correct time for surgical fixation. The early osteosynthesis appears to be ideal in order to avoid inflammatory processes and exuberant bony callus (9) although extended pulmonary contusions and lung or brain injury may contraindicate this approach. In the literature, the first information about chest wall reconstruction dates back to the early 1900s and focused on the technique of myoplasty using the latissimus dorsi (10). Titanium is the alloy of choice of plates, bars and screws, offering malleability, strength and easy applicability. Today, the discovery of prosthetic and biocompatible materials allowed the development of different surgical techniques for rib fractures stabilization, also managing particularly clinical conditions (11). Biocompatible synthetic materials are used also in association with rigid molded or titanium supports, muscle, musculocutaneous and omentum flaps, allowing the minimal adverse reactions.
Objective
The aim of this work is to report the state of the art on the reconstruction of the chest wall. We present this article in accordance with the Narrative Review reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-22-19/rc).
Methods
We carried out a review of the literature focusing the chest wall stabilization methods. The search has carried out using a combination of words, relevant MeSH terms and appropriate filters. As shown in Table 1, the strategy has developed in MEDLINE (via PubMed) between January 2010 and January 2022 and the following criteria are used: “chest trauma AND chest wall”. This research has allowed us to verify the most used techniques in the last period based on the possibility of the new materials available. A total of 1,385 results were obtained and 1,108 articles were identified after the duplicates and non-English were removed. Of these, 356 were relevant after reading the title and abstract. Subsequently only 214 were rated relevant after reading the full text (Figure 1). This step was performed independently by two investigators (surgeons experienced in the chest wall stabilization after trauma). In case of doubt, a third independent researcher (both senior surgeon and scientific researcher) intervened from the precedents. However, not being a systematic review but a wide review of the literature, we chosen to cite some older works as the indications provided are valid even today and support the most modern studies. After reading these articles we were able to evaluate the advantages and disadvantages of the various techniques. We evaluated exclusively the articles concerning the reconstruction of the chest wall after trauma (inclusion criterion), not considering the stabilization after resection of primary or secondary tumor (exclusion criterion).
Table 1
| Items | Specification |
|---|---|
| Date of search | October, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | Chest trauma AND chest wall |
| Timeframe | 2010–2022 |
| Inclusion and exclusion criteria | Inclusion: all types of studies that included stabilization techniques, in English |
| Selection process | Research conducted by two independent reviewers, discussion of results and elimination of duplicates and irrelevant work |
Key content and finding
Titanium plates and screws
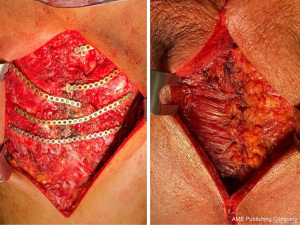
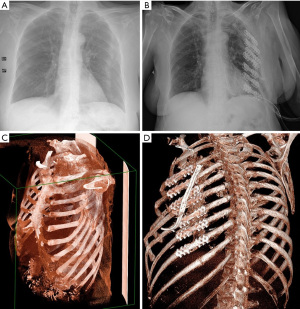
Titanium screws and plates have been a recognized method in thoracic surgery for about twenty years and mainly used for flail chest osteosynthesis (Figure 2). Titanium is an excellent prosthetic material: it is inert, resistant to corrosion and traction and compatible with all types of radiological and instrumental examinations. There are many different application systems whose use is often linked to the anatomical characteristics of lesions and manual skills of the surgeon (12-14). The needs must lead the shaping of plates, in order to adapt to the individual patient according to the ribs involved. There are two fundamental features of these devices: (I) corrosion resistance and elasticity, with coefficient of friction minimization and not interference with the physiological movement of the ribs, once the stiffness of the rib cage obtained; (II) quick and easy application method that allows a drastic reduction in surgical time (15,16). Some authors (17-19) compared outcomes between surgical stabilization with titanium plates and conservative management of trauma. The first group showed better results in terms of: (I) postoperative use of mechanical ventilation (4.5 vs. 16.0 days); (II) ICU stay (7 vs. 9 days); (III) total hospital length (12 vs. 19 days); (IV) percentage of complications such as pneumonia (4.55% vs. 25%); (V) need for reintubation (4.55% vs. 17.86%); (VI) home oxygen requirements (4.55% vs. 17.86%). The fast restoration of a good quality of life and of daily and working habits has an extremely positive economic and social impact (20). The plate breakage is rare but still described and probably linked to the different composition to the base titanium plate (21), the presence of pre-existing microfracture for an incorrect shaping of the device and the hyperactive delirium of the patient who carries out uncontrolled movements in the early postoperative time (22).
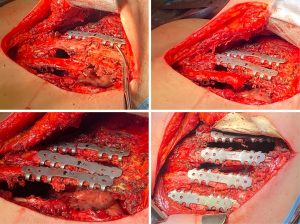
Judet’s struts and other types
Judet’s struts, used for a single rib fracture stabilization, are characterized by a linear base variable in length and width (from 12 to 24 mm) and by two or three pairs of hooks at the ends. The branches of the hooks show different angles in order to better adapt to the different anatomy of the upper and lower costal margins. After wide subperiosteal exposure of the fracture foci and the preventive correction of lesion, the strut application proceeds by tightening the hooks with special forceps. The advantages of this technique described in the seventies consist in the safety, ease and speed rib fixation (23). The disadvantages are as follows: (I) the need for a large thoracotomy to expose the injured chest wall; (II) longer operating times in case of multiple fracture foci; (III) chronic pain due to the crushing or entrapment of the neurovascular bundle; (IV) spontaneous rupture of the device if in steel (Figure 3), requiring the immediately removal to avoid vascular damage. The Sanchez-Lloret struts display straight and non-angled branches, equidistant along the plate; they meet the surgical indication for stabilization of several comminuted rib fractures (24). In addition to these classic devices, there are the plates made of 99% “pure” titanium which allow, compared to the various alloy steels, a greater thermal, mechanical and corrosive resistance and as well as greater lightness due to low density. Unfortunately, the plates with the hooks along their entire length are poorly adaptable to the morphology of the ribs. In fact, there is an overlap of the branches and a lifting of the extremities after modeling the horizontal component of the device and tightened the branches. This results in the non-adherence of the plate to the rib, with the possibility of seroma and displacement of the fracture stumps.
New struts in titanium
Device characterized by a straight support plate from which two or three pairs of hooks extend laterally, starting from each end (Figures 4,5). This plate is easily to shape in two dimensions (anteroposterior and superoinferior) according to the orientation and morphology of ribs, through the flexibility and deformability of all components. This involves the non-overlapping of the hooks after modeling due to the shape of plate that allows maintenance of the correct dimensional relationships. Consequently, the plate anchoring to the fractured ribs is easy, obtaining the quickly chest wall stabilization. The different angle of the vertical branches, according to the different anatomical characteristics of the rib edges (upper and lower), enhanced the sealing effect. In addition, there are two holes at the ends to simplify the fixation of several consecutive plates with screws in the case of comminuted fractures (16,22).
Bioresorbable materials
Unsintered hydroxyapatite (u-HA) particles/poly-L-Lactide (PLLA) (u-HA/PLLA) is a latest generation biocompatible and bioactive device already used in cranial, oral and maxillofacial surgery. There are sets of mini-plates and specific screws for the repair of flail chest and ribs. Mayberry et al. (25) showed the good clinical results, emphasizing the need to fix the rib with screws and cerclage. After 13 years, Oyamatsu et al. (26) proposed a U-shaped bioresorbable plate (SuperFIXSORB MX40) with ethibond 0/0 non-absorbable fixing points for the treatment of flail chest. Recently, Waseda et al. (27) described the same procedure in a severe osteoporotic octogenarian with serious flail chest due to a traffic accident, using resorbable Vicryl threads for fixation. The device would be partially reabsorbed at the 4-year follow-up and theoretically completely reabsorbed with another 2 years. This technique, applied in selected patients, requires more studies because the surgical stability failure leads to dislocation through the forces acting during the respiratory cycle (28).
Intramedullary components
The intramedullary stabilization method requires less surgical dissection; Kirschner wires, Adkins posts, steel wires and the Rehbein plate are the most frequently used. Although Kirschner wires displayed good results, the rotational instability or migration of the wires with local complications are still described (29). The Rehbein plate and the MatrixRIB plate with the rectangular intramedullary portion exploit a direct anchorage on the rib strut to prevent rotational instability (30,31). According to Botlang et al. (32) these systems are 48% stronger than Kirschner wires with reduced complications. These devices are clearly useful in the repair of ribs with limited access, such as the posterior ones. In the last period, the rib fractures stabilization has achieved with bioabsorbable intramedullary implants (33). Liovic et al. (34) described a novel technique with an intramedullary telescopic splint fixed by bone cement.
Mesh
Chest wall reconstruction with non-rigid materials is widely used. This technique involves the use of different devices, each with specific characteristics; the choice is evaluated case by case. Generally, the meshes adapt perfectly to any type of parietal defect reducing respiratory complications but involving to a risk of infections ranging from 10% to 25%; in these situations, removal may be required (35,36). Polypropylene, polyester and polytetrafluoroethylene (PTFE) are the most common non-absorbable materials. Easily extensible and applicable on the bone defect, these patches displayed good rigidity, protection and tolerance acting as a support for myoplasty. In particular, the DualMesh with bimaterial interface (one for the biocompatibility and the other for the tissue regeneration) seems to have excellent findings, reducing the risk of infection (37) ranged between 10% and 25% using Methyl Methacrylate (38). The collagen matrices collected from human or animal sources and processed for medical use that promote remodeling, neovascularization and exchange of the extracellular matrix with the tissues have proposed, with the biocompatibility advantages. D’Amico et al. (39) described parietal reconstructions associating biological implant and muscle flap, without major complications and patch infections. A polyglactin mesh has also used to avoid friction between the plate and the overlying skin after reconstruction (40). The titanium meshes are about 5 mm thick, perforated and with variable design. Tamburini et al. (41), in 26 chest wall tumors patients, used titanium mesh alone or associated with plates, with satisfactory short- and medium-term outcomes. Divisi et al. (42) applied the same device after wide sternal resection, with rapid recovery function of anterior chest wall. A further indication to the mesh is the thoracoabdominal injuries in which it is not possible to use the diaphragm for direct suturing (43). Gonfiotti et al. (44), in 10 trauma patients with a diameter of chest wall defects >5 cm, used a porcine-derived acellular dermal matrix associated with titanium plates for reconstruction. Overall survival was 100% after 30 days.
Discussion
The main objectives of the chest wall reconstruction are the respiratory function restoration, organ protection and pain reduction. In a multicenter study (45) we found that plates, screws or struts showed the same excellent results in the surgical stabilization of flail chest. The ideal timing for intervention is within 72 hours from trauma (16,45,46), if patients showed the hemodynamic and respiratory stabilization. In a previous study, we have already demonstrated the economic viability of titanium plate fixation in the sternal fracture and manubriosternal joint dislocation (46). Apaydin et al. (47) in a traumatic flail chest involving 7–8 costochondral joints in the right and 8 in left side and lower 1/3 of the sternum used: (I) 2 flat plates and 8 screws for the sternum; (II) 4 flat plates and 30 overall titanium screws for the ribs. Patient was extubated and mobilized on the first day. Evman et al. (48), in a patient who could not be weaned from mechanical ventilation after 14 days, carried out the surgical stabilization with titanium plates and screws allowing the extubation on third day and discharge on eighth day. The reconstruction of the chest wall with titanium plates and screws seems to have received unanimous consent from the literature (49,50). The patient’s clinical conditions, the morphology of the parietal defect and the experience of surgeon lead the choice of device (16). Dantis et al. (51) described a simple figure-eight suture with non-resorbable thread of rib fractures and apposition of polypropylene mesh. Patient needed the postoperative bronchoscopic cleaning of tracheobronchial tree and he was discharged from hospital after three weeks. In one month patient returned to work and one year follow-up shows no problem of respiratory dynamic. Tarng et al. (52) revealed chest wall repair with intramedullary titanium elastic nails (TENs) by video-assisted thoracoscopic surgery (VATS) and minimal thoracic incisions. All patients were successfully weaned from ventilators after an average of 3 days, with a shorter hospitalization than non-surgical patients, quickly returning to normal daily activities and work. Waseda et al. (27) stabilized the flail chest in a severe osteoporotic octogenarian using a biological resorbable plate and screw system in u-HA/PLLA with reinforcement by vicryl sutures. The 4-year check-up displayed the partial reabsorption of the fixing system, the completion of which will take an additional two years. Vacuum-assisted closure (VAC) therapy is a relatively new method of protecting sutures; the indications of which consist of infection or high infectious risk. Feng et al. (53), in a severe open trauma of the chest with multiple fractures, used the VAC therapy on the external site of the trauma after repair with titanium plates and screws. Lodin et al. (54) in 71 patients undergoing surgical chest stabilization with precontoured plates, systematically applied a local system of vacuum therapy (ciNPT: closed-incision negative pressure therapy). The study showed a reduction in both infection to 3% over a range of 2–20% (55) and in costs as also described by Hyldig et al. (56). In the reconstruction of the thoracic wall with large tissue defects needing greater stability, the use of prosthetic or biologic mesh associated with titanium plates and soft tissue flaps is described (57-59). Khan et al. (60), in a firearm chest injury with parietal defect measuring 10 cm × 15 cm, noticed excellent outcomes in term of stability and recovery function by rotation of the latissimus dorsi. However, there are many experiences on the use of the pectoralis major muscle (61), rectus abdominis (62) and omentum (63). Regarding the costs related to the surgical treatment, an interesting meta-analysis was carried out by Swart et al. (64). It is obvious that the cost of intervention is greater than conservative therapy ($23,682 vs. $8,629). However, the quality-adjusted life year (QALY) was equal to 32.60 vs. 30.84 respectively with a final ratio of $8,577/QALY. This finding, mainly due to the lower incidence of complications and shorter hospital stays, suggests that surgical treatment is to be preferred (65).
Conclusions
In the trauma chest wall reconstruction, the use of rigid devices is the quickest and safest way to achieve stability. Titanium is the preferred material due to inertia, chemical and physical properties and resistance to corrosion, evolving into lighter and more malleable alloys. Bioabsorbable implants are increasingly used although display limits of costs. Nonrigid mesh allows an excellent protection of the thoracic organs. Myoplasty is always advisable in order to re-establish the rigidity and functionality of the chest wall. VAC therapy is essential to avoid the risk of infection on the site of trauma. The best timing for intervention must be decided jointly between anesthesiologist and surgeon.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alessandro Gonfiotti) for the series “New Materials for Reconstruction in Thoracic Surgery” published in AME Surgical Journal. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-22-19/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-22-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-22-19/coif). The series “New Materials for Reconstruction in Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. DD serves as an unpaid Editorial Board Member of AME Surgical Journal from January 2021 to December 2024.The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jones KW. Thoracic trauma. Surg Clin North Am 1980;60:957-81. [Crossref] [PubMed]
- Milisavljević S, Spasić M, Arsenijevic M. Thoracic trauma. In: Cagini L. editor. Current Concepts in General Thoracic Surgery. InTech; 2012.
- Eghbalzadeh K, Sabashnikov A, Zeriouh M, et al. Blunt chest trauma: a clinical chameleon. Heart 2018;104:719-24. [Crossref] [PubMed]
- Lardinois D, Krueger T, Dusmet M, et al. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg 2001;20:496-501. [Crossref] [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-32. [Crossref] [PubMed]
- Mitchell JD. Blunt chest trauma: is there a place for rib stabilization? J Thorac Dis 2017;9:S211-7. [Crossref] [PubMed]
- Slater MS, Mayberry JC, Trunkey DD. Operative stabilization of a flail chest six years after injury. Ann Thorac Surg 2001;72:600-1. [Crossref] [PubMed]
- Cacchione RN, Richardson JD, Seligson D. Painful nonunion of multiple rib fractures managed by operative stabilization. J Trauma 2000;48:319-21. [Crossref] [PubMed]
- Wada T, Yasunaga H, Inokuchi R, et al. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: A propensity score-matched analysis. J Crit Care 2015;30:1227-31. [Crossref] [PubMed]
- Tensini I. Sopra il mio nuovo processo di amputazione della mammella. Gazzetta MedItal 1906;57:141-2.
- Crisci R, Divisi D. Chest wall surgical stabilization after thoracic trauma: indications and techniques. Shanghai Chest 2017;1:5.
- Mouton W, Lardinois D, Furrer M, et al. Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg 1997;45:242-4. [Crossref] [PubMed]
- Coonar AS, Qureshi N, Smith I, et al. A novel titanium rib bridge system for chest wall reconstruction. Ann Thorac Surg 2009;87:e46-8. [Crossref] [PubMed]
- Ng CS, Wong RH, Kwok MW, et al. Delayed fracture of MatrixRIB precontoured plate system. Interact Cardiovasc Thorac Surg 2014;19:512-4. [Crossref] [PubMed]
- Ramponi F, Meredith GT, Bendinelli C, et al. Operative management of flail chest with anatomical locking plates (MatrixRib). ANZ J Surg 2012;82:658-9. [Crossref] [PubMed]
- Divisi D, Barone M, Crisci R. Surgical management of flail chest: State of art and future perspectives. Curr Surg Rep 2017;5:21.
- Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care 2014;29:139-43. [Crossref] [PubMed]
- Althausen PL, Shannon S, Watts C, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma 2011;25:641-7. [Crossref] [PubMed]
- Schulz-Drost S, Grupp S, Pachowsky M, et al. Stabilization of flail chest injuries: minimized approach techniques to treat the core of instability. Eur J Trauma Emerg Surg 2017;43:169-78. [Crossref] [PubMed]
- Billè A, Okiror L, Campbell A, et al. Evaluation of long-term results and quality of life in patients who underwent rib fixation with titanium devices after trauma. Gen Thorac Cardiovasc Surg 2013;61:345-9. [Crossref] [PubMed]
- Stefani A, Nesci J, Morandi U. STRATOS™ system for the repair of pectus excavatum. Interact Cardiovasc Thorac Surg 2013;17:1056-8. [Crossref] [PubMed]
- Kim KT, Chang SW. An unexpected fracture of a titanium rib plate in a patient with traumatic brain injury. Trauma Case Rep 2019;24:100254. [Crossref] [PubMed]
- Judet R. Costal osteosynthesis Rev Chir Orthop Reparatrice Appar Mot 1973;59:334-5.
- Sánchez-Lloret J, Letang E, Mateu M, et al. Indications and surgical treatment of the traumatic flail chest syndrome. An original technique. Thorac Cardiovasc Surg 1982;30:294-7. [Crossref] [PubMed]
- Mayberry JC, Terhes JT, Ellis TJ, et al. Absorbable plates for rib fracture repair: preliminary experience. J Trauma 2003;55:835-9. [Crossref] [PubMed]
- Oyamatsu H, Ohata N, Narita K. New technique for fixing rib fracture with bioabsorbable plate. Asian Cardiovasc Thorac Ann 2016;24:736-8. [Crossref] [PubMed]
- Waseda R, Matsumoto I, Tatsuzawa Y, et al. Successful Surgical Fixation Using Bio-Absorbable Plates for Frail Chest in a Severe Osteoporotic Octogenarian. Ann Thorac Cardiovasc Surg 2019;25:336-9. [Crossref] [PubMed]
- Marasco SF, Sutalo ID, Bui AV. Mode of failure of rib fixation with absorbable plates: a clinical and numerical modeling study. J Trauma 2010;68:1225-33. [Crossref] [PubMed]
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg 1995;110:1676-80. [Crossref] [PubMed]
- Schüpbach P, Meier P. Indications for the reconstruction of the unstable thorax due to serial rib fractures and respiratory insufficiency. Helv Chir Acta 1976;43:497-502.
- Fitzpatrick DC, Denard PJ, Phelan D, et al. Operative stabilization of flail chest injuries: review of literature and fixation options. Eur J Trauma Emerg Surg 2010;36:427-33. [Crossref] [PubMed]
- Bottlang M, Helzel I, Long W, et al. Less-invasive stabilization of rib fractures by intramedullary fixation: a biomechanical evaluation. J Trauma 2010;68:1218-24. [Crossref] [PubMed]
- Nolasco-de la Rosa AL, Mosiñoz-Montes R, Matehuala-García J, et al. Unstable thorax fixation with bioabsorbable plates and screws. Presentation of some cases. Cir Cir 2015;83:23-8. [Crossref] [PubMed]
- Liovic P, Šutalo ID, Marasco SF. Fixation of a human rib by an intramedullary telescoping splint anchored by bone cement. Comput Methods Biomech Biomed Engin 2016;19:1297-305. [Crossref] [PubMed]
- Daigeler A, Druecke D, Hakimi M, et al. Reconstruction of the thoracic wall-long-term follow-up including pulmonary function tests. Langenbecks Arch Surg 2009;394:705-15. [Crossref] [PubMed]
- Thomas PA, Brouchet L. Prosthetic reconstruction of the chest wall. Thorac Surg Clin 2010;20:551-8. [Crossref] [PubMed]
- Nagayasu T, Yamasaki N, Tagawa T, et al. Long-term results of chest wall reconstruction with DualMesh. Interact Cardiovasc Thorac Surg 2010;11:581-4. [Crossref] [PubMed]
- Ng CS. Recent and Future Developments in Chest Wall Reconstruction. Semin Thorac Cardiovasc Surg 2015;27:234-9. [Crossref] [PubMed]
- D'Amico G, Manfredi R, Nita G, et al. Reconstruction of the Thoracic Wall With Biologic Mesh After Resection for Chest Wall Tumors: A Presentation of a Case Series and Original Technique. Surg Innov 2018;25:28-36. [Crossref] [PubMed]
- Rocco G, Fazioli F, Cerra R, et al. Composite reconstruction with cryopreserved fascia lata, single mandibular titanium plate, and polyglactin mesh after redo surgery and radiation therapy for recurrent chest wall liposarcoma. J Thorac Cardiovasc Surg 2011;141:839-40. [Crossref] [PubMed]
- Tamburini N, Grossi W, Sanna S, et al. Chest wall reconstruction using a new titanium mesh: a multicenters experience. J Thorac Dis 2019;11:3459-66. [Crossref] [PubMed]
- Divisi D, Tosi D, Zaccagna G, et al. Case Report: A New Tool for Anterior Chest Wall Reconstruction After Sternal Resection for Primary Or Secondary Tumors. Front Surg 2021;8:691945. [Crossref] [PubMed]
- Sekusky AL, Lopez RA. Diaphragm Trauma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 25, 2022.
- Gonfiotti A, Viggiano D, Vokrri E, et al. Chest wall reconstruction with implantable cross-linked porcine dermal collagen matrix: Evaluation of clinical outcomes. JTCVS Tech 2022;13:250-60. [Crossref] [PubMed]
- Divisi D, Mucilli F, Leonardo GD, et al. Plates versus struts versus an extracortical rib fixation in flail chest patients: Two-center experience. Injury 2021;52:235-42. [Crossref] [PubMed]
- Divisi D, Di Leonardo G, Crisci R. Surgical management of traumatic isolated sternal fracture and manubriosternal dislocation. J Trauma Acute Care Surg 2013;75:824-9. [Crossref] [PubMed]
- Apaydın T, Arapi B, Başaran C. Surgical reconstruction of traumatic flail chest with titanium plaques. Int J Surg Case Rep 2018;50:72-4. [Crossref] [PubMed]
- Evman S, Kolbas I, Dogruyol T, et al. A Case of Traumatic Flail Chest Requiring Stabilization with Surgical Reconstruction. Thorac Cardiovasc Surg Rep 2015;4:8-10. [Crossref] [PubMed]
- Brown SR, Fernandez C, Bertellotti R, et al. Blunt rupture of the thoracic duct after severe thoracic trauma. Trauma Surg Acute Care Open 2018;3:e000183. [Crossref] [PubMed]
- El-Akkawi AI, de Paoli FV, Andersen G, et al. A case of severe flail chest with several dislocated sterno-chondral fractures. Int J Surg Case Rep 2019;65:52-6. [Crossref] [PubMed]
- Dantis K, Brahmachari S, Raju A, et al. An innovative technique of chest wall stabilization and reconstruction in traumatic flail chest: The figure-of-eight suture with polypropylene mesh and musculofascial flap. Chin J Traumatol 2022;25:122-4. [Crossref] [PubMed]
- Tarng YW, Liu YY, Huang FD, et al. The surgical stabilization of multiple rib fractures using titanium elastic nail in blunt chest trauma with acute respiratory failure. Surg Endosc 2016;30:388-95. [Crossref] [PubMed]
- Feng K, Yin D, Zheng W, et al. Treatment of open chest rib fractures with the matrix rib internal fixation system: A case report. Medicine (Baltimore) 2019;98:e15683. [Crossref] [PubMed]
- Lodin D, Florio T, Genuit T, et al. Negative Pressure Wound Therapy Can Prevent Surgical Site Infections Following Sternal and Rib Fixation in Trauma Patients: Experience From a Single-Institution Cohort Study. Cureus 2020;12:e9389. [Crossref] [PubMed]
- Thiels CA, Aho JM, Naik ND, et al. Infected hardware after surgical stabilization of rib fractures: Outcomes and management experience. J Trauma Acute Care Surg 2016;80:819-23. [Crossref] [PubMed]
- Hyldig N, Birke-Sorensen H, Kruse M, et al. Meta-analysis of negative-pressure wound therapy for closed surgical incisions. Br J Surg 2016;103:477-86. [Crossref] [PubMed]
- Oostendorp SEV, Buijsman R, Zuidema WP. Cough-induced nonunion rib fractures and herniation: surgical repair and review. Asian Cardiovasc Thorac Ann 2018;26:416-8. [Crossref] [PubMed]
- McNickle AG, Dickhudt T, Vega JA, et al. Emergent chest wall reconstruction for an incarcerated pulmonary hernia. J Trauma Acute Care Surg 2018;85:820-2. [Crossref] [PubMed]
- Aladaileh M, O'Driscoll-Collins A, O'Keeffe F, et al. Traumatic thoracoabdominal hernia repair using a novel chest-wall reconstruction technique: a case report. Ann R Coll Surg Engl 2020;102:e4-6. [Crossref] [PubMed]
- Khan NU, Ahmed Z, Malik F, et al. Emergency chest wall reconstruction in open pneumo-thorax from gunshot chest: A case report. J Pak Med Assoc 2020;70:S118-21.
- Opoku-Agyeman J, Matera D, Simone J. Surgical configurations of the pectoralis major flap for reconstruction of sternoclavicular defects: a systematic review and new classification of described techniques. BMC Surg 2019;19:136. [Crossref] [PubMed]
- Daigeler A, Simidjiiska-Belyaeva M, Drücke D, et al. The versatility of the pedicled vertical rectus abdominis myocutaneous flap in oncologic patients. Langenbecks Arch Surg 2011;396:1271-9. [Crossref] [PubMed]
- Jurkiewicz MJ, Arnold PG. The omentum: an account of its use in the reconstruction of the chest wall. Ann Surg 1977;185:548-54. [Crossref] [PubMed]
- Swart E, Laratta J, Slobogean G, et al. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J Orthop Trauma 2017;31:64-70. [Crossref] [PubMed]
- Hojski A, Xhambazi A, Wiese MN, et al. Chest wall stabilization and rib fixation using a nitinol screwless system in selected patients after blunt trauma: long-term results in a single-centre experience. Interact Cardiovasc Thorac Surg 2022;34:386-92. [Crossref] [PubMed]
Cite this article as: Divisi D, De Vico A, Zaccagna G, Marella A, De Sanctis S, Crisci R. Reconstructive options of the chest wall after trauma: a narrative review. AME Surg J 2023;3:17.




