Appendiceal tumour mimicking ovarian malignancy: when to think outside the box
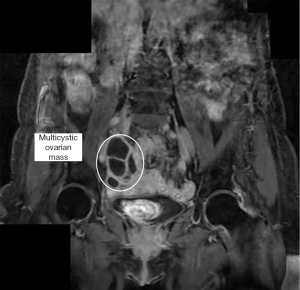
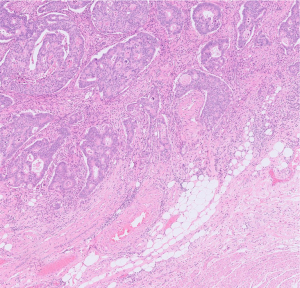
A 69-year-old woman was referred to the gynaecological oncology team due to vague abdominal pain, lethargy, and appetite loss over the previous month. Tumour markers of carcinoembryonic antigen (CEA) 3.3 micrograms (normal), cancer antigen (CA) 19-9 3U (normal), and CA-125 91 IU/mL (raised) were most suggestive of ovarian malignancy. A computerised tomography (CT) thorax abdomen pelvis scan to look for the cause of the elevated CA-125 showed a right ovarian mass with potential involvement of a dilated appendix and adjacent small bowel. Follow-up magnetic resonance (MR) imaging of the pelvis (Figure 1) also showed the presence of this complex right ovarian mass. As a result of the ambiguities in the imaging, despite the normal CEA, exploratory laparoscopy staging was undertaken. The laparoscopy further raised the suspicion of an appendicular tumour, due to a complex tubo-ovarian appendicular mass engulfed by surrounding structures (Figure 2). A pre-operative colonoscopy identified one 15-mm sessile polyp present in the ascending colon near the ileocaecal valve, but the appendiceal orifice was clear. The identified polyp was not biopsied.
In a joint gynaecological oncology and colorectal operation, the patient underwent midline laparotomy, en bloc total abdominal hysterectomy, bilateral salpingo-oophorectomy and extended right hemicolectomy, with infracolic omentectomy, appendicectomy, and primary anastomosis without diversion. Clear margins were achieved with no residual disease.
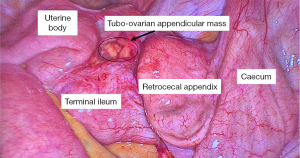
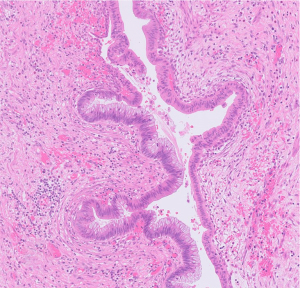
Histopathology diagnosis confirmed a low-grade appendiceal mucinous neoplasm (Figure 3) and an incidental pT1 N0 adenocarcinoma at the ileocaecal valve (Figure 4).
The patient has recovered fully with no relapse of symptoms 1 year post-operation. She will have annual CT scans, tumour markers surveillance, and 5-yearly colonoscopies.
Acknowledgments
The authors acknowledge the support of the following colleagues in preparation of the images: Dr. Aniko Rendek from Department of Cellular Pathology, Oxford University Hospital NHS Trust and Dr. Zoe Traill from Department of Radiology, Oxford University Hospital NHS Trust.
Funding: None.
Footnote
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-22-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-22-38/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent has been obtained from the patient for publication of this Clinical Picture report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Yu Z, Smyth SL, Soleymani majd H. Appendiceal tumour mimicking ovarian malignancy: when to think outside the box. AME Surg J 2023;3:41.