
Innovative approaches to preoperative care including feasibility, efficacy, and ethical implications: a narrative review
Introduction
Background
Traditional preoperative care consists of a series of evaluations and interventions aimed at optimizing surgical outcomes. These usually include patient interviews, diagnostic tests, and preoperative fasting protocols. While these methods have demonstrated utility, advances in technology and our understanding of human physiology and psychology suggest that we may be on the cusp of a paradigm shift in preoperative care. In fact, health systems are already implementing novel approaches such as artificial intelligence (AI) machine learning applications in preoperative risk assessment which has been shown to be more utilitarian than conventional risk assessment tools (e.g., American Society of Anesthesiologists Physical Status) (1,2). A holistic approach to preoperative care has also seen a steady rise in clinical trials and is showing promising results in improving postoperative outcomes (3).
Rationale and knowledge gap
Emerging literature has highlighted that pre-operative hematological, renal, and nutritional statuses are some of the vital aspects to both outcomes of an operation and recovery in the post-surgical period (4,5). Optimizing these health components may also aid in reducing morbidity and mortality in the intra-operative and post-surgical period. In particular, the elderly population presents as a vulnerable group that require further evaluation including cognition, pre-operative or pre-morbid function and frailty for operative management and post-operative recovery (6). As such, the need for novel approaches, as those of multidisciplinary and holistic care, are more pertinent now than ever as they complement the primary clinicians’ work in navigating through the complexities of preoperative care. Currently, the existing narrative reviews on preoperative care focus on specific aspects such as pain management and geriatric populations. However, a comprehensive examination of multiple factors has not been done yet. Consequently, this review aims to consolidate and synthesize several elements within the realm of preoperative care.
Objective
The combination of technological integrations with holistic approaches in risk assessment, patient education, and multidisciplinary management appear to offer distinct advantages over conventional methodologies. These innovations are aimed at decreasing preoperative length of stay and improving surgical flow, ultimately decreasing overall healthcare costs, and improving patient outcomes (7). With these aims in mind, emerging approaches are proactive, with the potential for many techniques to be implemented prior to or separate from patient admission(s). The objectives of this review are to explore these emerging strategies in preoperative care, assessing their feasibility, efficacy, and ethical implications. The ultimate aim is to provide a summary of feasible and effective strategies for clinicians and health systems to consider adopting. We present this article in accordance with the Narrative Review reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-23-41/rc).
Methods
A comprehensive literature search was performed in multiple databases including PubMed, Scopus, Web of Science, and Cochrane Library. The search spanned from September 2013 to August 2023. Two authors (K.J. and M.V.) independently conducted the search using keywords: “preoperative care”, “preoperative management”, “innovative approaches”, “risk assessment”, “patient education”, and “technological integration”. The inclusion criteria encompassed (I) peer-reviewed articles, clinical trials, reviews, and meta-analyses relevant to innovative strategies in preoperative care and (II) English language. Articles not completely accessible, redundant publications, and editorial articles were excluded. Identified articles were subsequently screened by title and abstract and assessed for eligibility based on their relevance to the aim of the review. Articles focusing on dated management strategies and those without substantial discussion regarding novel approaches were excluded on a case-by-case basis. Discrepancies were resolved through discussion and, where needed, a third author’s opinion (I.S.) was sought. A summary of the search strategy is shown in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 18 September 2023 |
| Databases and other sources searched | PubMed, Scopus, Web of Science, and Cochrane Library |
| Search terms used | “Preoperative care”, “preoperative management”, “innovative approaches”, “risk assessment”, “patient education”, and “technological integration” |
| Timeframe | September 2013 to August 2023 |
| Inclusion and exclusion criteria | Inclusion: (I) peer-reviewed articles, clinical trials, reviews, and meta-analyses; (II) English language |
| Exclusion: articles not completely accessible, redundant publications, and editorial articles | |
| Selection process | Two authors (K.J. and M.V.) independently conducted the selection of articles. In discrepancies, a discussion was held and where needed, a third author’s (I.S.) opinion was sought to achieve consensus |
An example of a detailed search strategy of a database (PubMed) is shown in Table S1. Seven hundred and twenty-six total results were found.
Results
Innovative approaches can be classified into two themes: personalized holistic care and technological integration (Figure 1). Despite this categorization, both themes function synergistically and were studied concomitantly.
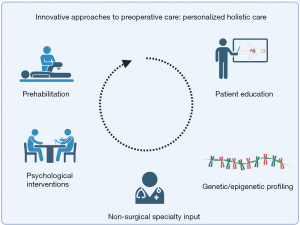
Personalized holistic care
As we gain a greater appreciation for patient needs from a holistic perspective, there are now more opportunities than ever for medical specialists and allied health staff to get involved with preoperative patient care. This multidisciplinary approach aims to provide medical, physical, psychological, and emotional care. Innovations in risk assessment, patient education, and psychological intervention are poised to optimize patient outcomes by affording clinicians from various health disciplines to tailor assessments and provide in-depth, individualized care plans.
Non-surgical specialty input
Non-surgical input refers to the involvement of non-surgical specialists in the care of surgical patients. This often entails multidisciplinary teams with the overall goal of optimizing patient health during the perioperative period. Pain is a prevalent and often complex complaint that may be encountered during the perioperative period. In pain medicine, personalized care is being achieved through the integration of pharmacogenomics as seen in enhanced recovery after surgery (ERAS) programs. For surgical patients who are exposed to new medications for the first time, pharmacogenomic information may offer an opportunity to reduce adverse drug events and optimize drug efficacy during the perioperative period (8). Additionally, tools like PROMIS and CHOIR are being employed to capture patient-reported outcomes, refining the perioperative care experience (9). The Perioperative Pain Program at Johns Hopkins Hospital provides continuous care from pre- to post-surgery with a collaborative team of specialists. This integrated approach promotes patient-centered care in which individualized assessments of pain-experiences during the preoperative have been shown to promote improved patient satisfaction with surgical procedures (10). Such advancements and comprehensive approaches herald a new era in perioperative pain management, paving the way for a personalized and enhanced patient experience across healthcare institutions.
Further multidisciplinary teams that may be involved in patient care during the perioperative period may include anesthetists, surgeons, nurses, geriatricians, pharmacists, chaplains, and more (11). Particularly for high-risk or comorbid patients such as the elderly, comprehensive assessment facilitates optimal management, decreasing adverse events and improving patient outcomes (12). In the elderly population, a comprehensive geriatric assessment can be vital to identify and pre-operatively manage physiological decline, co-morbidities and geriatric syndromes and can be aided by specialist geriatricians (e.g., dementia, delirium, frailness, incontinence, etc.) (13-15). In another unique population, patients seeking cosmetic procedures may benefit from psychiatric assessments, as they experience an increased burden of psychiatric conditions such as body dysmorphia (16). The appropriate identification and management of patients with psychopathology can prevent unindicated procedures, improve post-operative outcomes such as patient satisfaction, and optimize patient health in the long term (16,17).
Psychological interventions
The benefits of psychological intervention have also been demonstrated in the preoperative period for other surgeries, where it stands to benefit the post-operative pain experience and improve patient experience. Psychological interventions may take form as placebo mechanisms which have been shown to improve disability and quality of life post-surgery. This can be done through pre-operative counseling sessions with psychologists either face-to-face or by telehealth. In these sessions, patients are encouraged to develop a vision about their daily life after surgery. This plants an expectation that patients will aim for so as to achieve their desired quality of life in an expedited time (18). In the realm of pain management, placebo mechanisms have been significant in reducing post-operative pain by the overestimation of analgesic efficacy in pre-operative counseling sessions (19). Other psychological-based interventions may involve cognitive behavioral therapy (CBT) and mindfulness-based interventions. Preoperative anxiety is an important issue for patients. Validated scoring systems such as the Amsterdam Preoperative Anxiety and Information Scale (APAIS) have been developed as practical methods to assess for patient anxiety and its implementation during the preoperative period is poised to benefit patient satisfaction and functional outcomes (20). Literature suggests that CBT may be effective in reducing preoperative anxiety in addition to pain (21). By helping patients identify and reframe irrational beliefs and thought patterns associated with surgical procedures, CBT can mitigate psychological distress, and decrease pain perception. Mindfulness-based strategies have shown promise in lowering preoperative stress and pain by enhancing patients’ ability to manage these symptoms (22,23). Techniques such as focused breathing and meditation are taught to patients, enabling them to achieve improved emotional regulation. Recent studies have shown that implementing mindfulness-based interventions preoperatively and continuing them through the course of bariatric surgery can lead to improved psychological health and retention of long-term weight loss, which themselves are among the major goals of bariatric procedures (24,25).
In the management of preoperative anxiety, a prevalent condition among those awaiting surgery, music therapy may work synergistically with pharmacologic interventions such as sedatives and anxiolytics used in traditional preoperative care. This potentially reduces their administration and therefore the adverse reactions (e.g., drowsiness, breathing difficulties, prolonged postoperative recovery, drug interactions, etc.) associated with them. A large-scale systematic review has found music therapy to have a significant beneficial effect on preoperative anxiety, reporting an anxiety reduction in the Stait-Trait Anxiety Inventory by more than 5.72 units (P<0.00001) (26).
Prehabilitation
Prehabilitation is a preoperative conditioning intervention that aims to prevent or reduce surgery-related functional decline and adverse outcomes. This employs physiotherapists, occupational therapists, and dieticians to promote optimal exercise, daily function, and nutrition before surgery. While definitive trials are pending, initial studies suggest it enhances preoperative health and increases post-surgery recovery speed, risk of infections, wound healing complications, and respiratory issues (27-30). This proactive strategy towards managing surgical patients is gaining global traction for its potential benefits, improved patient outcomes, and reduced hospital length of stay. Ongoing trials will determine its full impact, but current data suggests prehabilitation is a cost-effective and transformative advancement in perioperative care (31,32).
Patient education
Education empowers patients with tangible knowledge and strengthens their relationship with healthcare services by increasing their involvement with their own care. The importance of patient education in preoperative care is indisputable, with current literature highlighting its role in reducing anxiety and improving patient compliance (33). The advent of digital technology and integrations with telehealth and virtual reality (VR) platforms has transformed this area. VR platforms offer an immersive educational experience by simulating the surgical environment. This not only familiarizes patients with the procedure but also reduces preoperative anxiety (33). Additionally, mobile applications are becoming increasingly sophisticated, offering interactive features such as real-time chat support, video tutorials, and symptom tracking (34). These platforms also enable the dissemination of patient-specific educational content tailored to individual needs and preferences.
Genetics/epigenetic profiling
The development of non-invasive markers to aid in the identification and subsequent risk stratification of malignant lesions is of urgent priority (35). (Epi)genetic profiling involves utilizing genetic and epigenetic markers to identify and differentiate between lesions that may lack specific biomarkers and present with indistinct phenotype (36). These techniques are finding increasing application in the clinical setting, including in that of perioperative care. In 2022, Meagher et al. (36) analyzed clinicopathologic and gene-expression data from patients during the preoperative period to identify prognostic and diagnostic features of ovarian lesions. They found significant associations between specific gene expression and overall survival, and were able to identify receptor subtypes that could be subsequently targeted with adjuvant treatment in 26% of patients with mucinous ovarian carcinoma. Epigenetic analyses have also been implemented to predict the risk of premalignant progression in breast lesions, providing clinicians and patients alike with important information that can help them make an informed decision and avoid under- or overtreatment (37). Issues regarding data privacy with (epi)genetic analyses is a developing subject. As these technologies improve, careful oversight will be necessary to ensure that practical applications do not undermine the medical integrity.
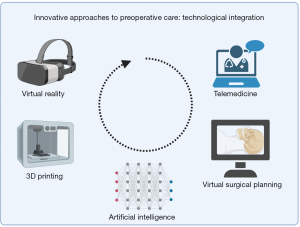
Technological integration
Ongoing technological innovations and integrations (Figure 2) are both exciting and challenging. Preoperative care is rapidly evolving due to technological advances and an expanding understanding of patient needs. AI, VR and augmented reality (AR) technologies, telehealth, three-dimensional (3D) printing, and virtual surgical planning (VSP) leverage rapidly developing computing powers to capture, process, and present crucial information to patients and clinicians alike (2,33,34). AI and AI-integrated technologies have undergone unprecedented expansion within surgical care in recent years. However, concerns regarding data quality, privacy, and ethical considerations currently hinder widespread integration into patient management strategies (38).
VR and AR technologies
In addition to the aforementioned VR technologies impacting preoperative patient education, AR offers distinct advantages for surgeons when planning their procedures (39,40). AR harnesses the power of wearable sensors and remote monitoring systems which are now capable of capturing a broad range of physiological data, which can be subsequently processed and superimposed onto physical or virtual anatomical structures. These technologies are used for VSP, where advancements in computer hardware and software help streamline the preoperative process. In addition to helping clinicians visualize patient-specific anatomy whilst planning procedures, this technology enables clinicians to simulate surgeries, predict effective approaches, and solve potential complications before working on patients (41). This reduces intraoperative uncertainty and has been used to great effect in fields that have traditionally relied on resource-intensive surgical modeling, such as craniofacial surgery, where it improves operative efficiency and increases the accuracy of reconstructions (41,42). Conventional stone-modeling requires extensive time-commitment for patients, technicians, and clinicians for radiographic acquisition/analysis, moulding, model fabrication, and splint preparation. VSP simplifies these processes and in doing so reduces the opportunities for inaccuracies to be potentiated.
Telemedicine
Telemedicine platforms harness digital power to expanded the reach of preoperative consultation services, especially crucial in rural areas or in situations where in-person visits are not possible, such as during pandemics (43). The use of telemedicine to implement preoperative evaluations has led to increased patient and provider satisfactions, and lower rates of same-day procedure cancellations as compared with face-to-face appointments (44,45). Additionally, telemedicine expands the breadth of other medical specialty and allied health input through the convenience it can provide, enabling holistic care (46). Telemedicine was also found to improve workflow efficiency, hastening the process of patients being reviewed in pre-admission clinics and expediting surgery (47). Internet-delivered pre-operative preparation programs have been shown to be cost-effective, helping address another drawback of traditionally delivered preoperative care (48).
AI and machine learning
AI algorithms and its branches such as machine learning are being explored for their ability to analyze large datasets, potentially uncovering new predictors of surgical risk (2). AI is being implemented to benefit preoperative patient care in oncologic surgery, where it is used to predict histopathology and guide subsequent treatment selection (49-51). There exist opportunities to integrate AI with the aforementioned strategies aimed at optimizing preoperative management such as the use of (epi)genetic markers for lesion identification. In 2022, Bahado-Singh et al. reported the accurate detection of epithelial ovarian cancer using AI to analyze epigenetic markers from cell-free tumor DNA (cftDNA) samples (35). This exemplifies the power of leveraging novel preoperative strategies with one another and opens the door to further collaborations between AI and (epi)genetic marker use.
3D printing
3D printing has evolved considerably since its first applications in the medical field in the early 2000s (52). Its implementation in the preoperative setting involves utilizing data from medical images to produce detailed, free-form, patient-specific models in a layer-by-layer fashion (53). These models aid clinicians to visualize the morphology of anatomic structures such as cardiac defects, and help facilitate the planning of complex procedures (54). Employing these models during the preoperative period has been associated with improved operative outcomes and decreased operating times, when compared with standard preoperative planning (55). Developments in imaging acquisition, processing, and printing techniques continue to propel this field forward. Recent improvements in echocardiographic (ECHO) imaging have made it possible to create cardiac models from ECHO data, affording opportunities to characterize cardiac defects without the radiation of computed tomography or the expense of magnetic resonance imaging (56).
Discussion
The landscape of perioperative care has been undergoing a remarkable evolution, with a focus on improving patient outcomes and experiences through increasingly individualized and participative care. Targeted assessment and patient education techniques empower patients and promote perioperative wellness from a holistic perspective. Recent advancements in preoperative pain management, as evidenced by the shift towards patient-centered care in ERAS programs, showcase this trend. The integration of pharmacogenomics to tailor pain management strategies and the use of patient-reported outcomes tools, like PROMIS and CHOIR, signify an era of personalized medicine, as evidenced by programs such as the Perioperative Pain Program at Johns Hopkins Hospital (8,9). In tandem with these advancements, the rise of prehabilitation brings a proactive approach to surgical preparation, harnessing exercise, nutrition, and mental support. The early evidence indicates that prehabilitation not only bolsters preoperative health but also mitigates postoperative complications (27-30). As research progresses, these pioneering approaches to perioperative care are poised to become standard practices, setting the stage for enhanced surgical outcomes and a revolutionized patient experience.
Our literature search also revealed an exciting forefront of technologies that are being integrated into preoperative patient care. Rigorous, multi-disciplinary research is needed to further evaluate the efficacy, ethics, and economics of these emerging strategies. The advancement and implementation of (epi)genetic marker technologies for lesion identification and risk assessment offers clinicians the opportunity to provide individualized preoperative patient care in a relatively noninvasive fashion in the outpatient setting. As our understanding of gene expression and sequencing expands, these technologies will likely find more and more application in various medical fields. This technology should not, however, be used without oversight. Along with advancements in data storage and computing powers, ethical issues regarding incidental findings, data privacy, consent, and potential misuse must be considered and call for regulatory measures (57,58).
AI in surgery is a burgeoning topic. Machine learning, a subset of AI, is increasingly being used for predictive analytics in risk stratification adds granularity to traditional models, enabling more individualized care plans. For instance, machine learning algorithms are capable of synthesizing multi-dimensional patient data, including lifestyle factors, genomics, and past medical histories, to predict postoperative complications with remarkable accuracy (2). While various AI integrations promise improved preoperative care, they come with challenges. There exist concerns about algorithmic bias in AI applications and the development of ethical guidelines will be necessary to ensure equitable care and prevent the exacerbation of health disparities (38).
Telemedicine and remote monitoring have proven particularly valuable in the current pandemic scenario, facilitating cost-efficient preoperative consultations without exposing patients to infection risks (43,48). However, the quality of care through telehealth services, especially for complex preoperative assessments that would benefit from a physical examination component, remains under scrutiny (59).
VR simulations and mobile health apps not only offer educational value but also serve as platforms for remote patient monitoring and real-time healthcare provider interactions (33,34). The adaptability of these platforms allows for a truly personalized patient education strategy. However, the digital divide could render these advances inaccessible to underserved communities or older adults who are not tech-savvy.
Another consideration of VR simulation is the employment of VSP. Despite its evident utility and the benefits it may hold for surgeons at various stages of their careers, it should not be utilized at the cost of developing physical surgical skills. As technologies are integrated into the surgical fields and surgeons rely increasingly on advancements such as VSP, it will become imperative for programs to preserve hands-on training hours for junior surgeons. Laparoscopic approaches to abdominal surgeries, for example, have long overtaken open techniques which are subsequently becoming a diminishing art with the potential implications for training surgeons who should be exposed to various techniques in order to develop a robust skillset (60). With this in mind, cognizance of the potential for technological advancements in preoperative strategies to negatively impact traditional skill sets should be maintained.
Cost remains a significant hurdle when considering the clinical application of these technologies. Although the implementation of well-established applications such as those seen in telehealth have been shown to offer cost efficient alternatives to traditional preoperative care (48), financial barriers could hinder the integration of newer technologies. Advanced technologies, particularly those offering personalized approaches, often come at a high price, which raises questions about their long-term sustainability and scalability, particularly in resource-limited settings (61). In addition to the costs of the software and hardwares themselves, the adaptation of these technologies requires comprehensive training for healthcare professionals, another logistical and financial challenge. However, as the use of technologies such as 3D printing are becoming widespread, affordability is improving. User competence is poised to increase with uptake, which will likely encourage further integrations and innovations within the surgical fields.
This comprehensive review presents a nuanced and detailed exploration of the innovative approaches in perioperative care, emphasizing personalized holistic care and technological integration. The strength of the review lies in its extensive scope, covering a broad range of interventions from psychological strategies and prehabilitation techniques to cutting-edge technological advancements like AI and 3D printing. It provides a holistic view of current and potential practices, offering a rich synthesis of multidisciplinary approaches that highlight the synergy between personalized care and technological innovation. Furthermore, the review effectively illustrates the potential for these innovations to revolutionize patient outcomes, emphasizing the shift towards patient-centered care and the integration of various specialties. However, the review also exhibits certain limitations. The breadth of topics, while comprehensive, may lead to a superficial treatment of complex individual subjects due to the inherent constraints of the review format. Additionally, the quality of the literature included spans a wide array, encompassing everything from early trials and preliminary studies to more established research. This variation in the evidence base necessitates a cautious interpretation of the findings, particularly concerning the newer, less-validated technologies. The review could benefit from a more critical appraisal of the strengths and weaknesses of individual studies, including considerations of study design, sample size, and potential biases. This would provide a more nuanced understanding of the reliability and applicability of the reported innovations. Overall, while the review offers an informative and broad overview of advancements in perioperative care, it would be enhanced by a more detailed analysis of the literature quality and a more critical examination of the individual studies’ methodologies and findings.
Conclusions
In summary, the emerging innovations in preoperative care offer significant promise but come with a complex array of challenges that span ethics, cost-effectiveness, and quality of care. As we move towards a more technologically integrated healthcare system, it is imperative to address these challenges through multidisciplinary research and ethical governance.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-23-41/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-23-41/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-23-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li YY, Wang JJ, Huang SH, et al. Implementation of a machine learning application in preoperative risk assessment for hip repair surgery. BMC Anesthesiol 2022;22:116. [Crossref] [PubMed]
- Nguyen A, Vanderbeek C, Herford AS, et al. Use of Virtual Surgical Planning and Virtual Dataset With Intraoperative Navigation to Guide Revision of Complex Facial Fractures: A Case Report. J Oral Maxillofac Surg 2019;77:790.e1-790.e17. [Crossref] [PubMed]
- Xie YH, Xie HT, Wang TS, et al. Perioperative holistic care more significantly reduces levels of anxiety and depression of pituitary tumor patients versus conventional care. Medicine (Baltimore) 2019;98:e14411. [Crossref] [PubMed]
- Gillis C, Wischmeyer PE. Pre-operative nutrition and the elective surgical patient: why, how and what? Anaesthesia 2019;74:27-35. [Crossref] [PubMed]
- Pichette M, Liszkowski M, Ducharme A. Preoperative Optimization of the Heart Failure Patient Undergoing Cardiac Surgery. Can J Cardiol 2017;33:72-9. [Crossref] [PubMed]
- Wozniak SE, Coleman J, Katlic MR. Optimal Preoperative Evaluation and Perioperative Care of the Geriatric Patient: A Surgeon's Perspective. Anesthesiol Clin 2015;33:481-9. [Crossref] [PubMed]
- Lee A, Kerridge RK, Chui PT, et al. Perioperative Systems as a quality model of perioperative medicine and surgical care. Health Policy 2011;102:214-22. [Crossref] [PubMed]
- Jhun EH, Apfelbaum JL, Dickerson DM, et al. Pharmacogenomic considerations for medications in the perioperative setting. Pharmacogenomics 2019;20:813-27. [Crossref] [PubMed]
- Chen Q, Chen E, Qian X. A Narrative Review on Perioperative Pain Management Strategies in Enhanced Recovery Pathways-The Past, Present and Future. J Clin Med 2021;10:2568. [Crossref] [PubMed]
- Hanna MN, Speed TJ, Shechter R, et al. An Innovative Perioperative Pain Program for Chronic Opioid Users: An Academic Medical Center's Response to the Opioid Crisis. Am J Med Qual 2019;34:5-13. [Crossref] [PubMed]
- Staheli B, Rondeau B. Anesthetic Considerations in the Geriatric Population. 2023.
- Partridge JS, Harari D, Martin FC, et al. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia 2014;69:8-16. [Crossref] [PubMed]
- Pang CL, Gooneratne M, Partridge JSL. Preoperative assessment of the older patient. BJA Educ 2021;21:314-20. [Crossref] [PubMed]
- Naji A, Stolin GB, Ahmed A, et al. Preoperative Assessment of Geriatric Patients Undergoing Elective Intracranial Surgery. Cureus 2020;12:e12284. [Crossref] [PubMed]
- Partridge JSL, Healey A, Modarai B, et al. Preoperative comprehensive geriatric assessment and optimisation prior to elective arterial vascular surgery: a health economic analysis. Age Ageing 2021;50:1770-7. [Crossref] [PubMed]
- van Essen P, Keillor N, Long R, et al. Surgeon-driven preoperative psychiatric evaluation of plastic surgery patients. Australasian Journal of Plastic Surgery 2021;4:85-92. [Crossref]
- Bascarane S, Kuppili PP, Menon V. Psychiatric Assessment and Management of Clients Undergoing Cosmetic Surgery: Overview and Need for an Integrated Approach. Indian J Plast Surg 2021;54:8-19. [Crossref] [PubMed]
- Rief W, Shedden-Mora MC, Laferton JA, et al. Preoperative optimization of patient expectations improves long-term outcome in heart surgery patients: results of the randomized controlled PSY-HEART trial. BMC Med 2017;15:4. [Crossref] [PubMed]
- Vase L, Wartolowska K. Pain, placebo, and test of treatment efficacy: a narrative review. Br J Anaesth 2019;123:e254-62. [Crossref] [PubMed]
- Celik F, Edipoglu IS. Evaluation of preoperative anxiety and fear of anesthesia using APAIS score. Eur J Med Res 2018;23:41. [Crossref] [PubMed]
- Everitt HA, Landau S, O'Reilly G, et al. Assessing telephone-delivered cognitive-behavioural therapy (CBT) and web-delivered CBT versus treatment as usual in irritable bowel syndrome (ACTIB): a multicentre randomised trial. Gut 2019;68:1613-23. [Crossref] [PubMed]
- Bishop SR, Lau M, Shapiro S, et al. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice 2004;11:230-41.
- Hymowitz G, Hasan F, Yerramalli G, et al. Mindfulness-Based Interventions for Surgical Patients and Impact on Postoperative Outcomes, Patient Wellbeing, and Satisfaction. Am Surg 2022; Epub ahead of print. [Crossref] [PubMed]
- Himes SM, Grothe KB, Clark MM, et al. Stop regain: a pilot psychological intervention for bariatric patients experiencing weight regain. Obes Surg 2015;25:922-7. [Crossref] [PubMed]
- Mushquash AR, McMahan M. Dialectical behavior therapy skills training reduces binge eating among patients seeking weight-management services: preliminary evidence. Eat Weight Disord 2015;20:415-8. [Crossref] [PubMed]
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev 2013;2013:CD006908. [Crossref] [PubMed]
- Durrand J, Singh SJ, Danjoux G. Prehabilitation. Clin Med (Lond) 2019;19:458-64. [Crossref] [PubMed]
- McIsaac DI, Gill M, Boland L, et al. Prehabilitation in adult patients undergoing surgery: an umbrella review of systematic reviews. Br J Anaesth 2022;128:244-57. [Crossref] [PubMed]
- Snow R, Granata J, Ruhil AV, et al. Associations between preoperative physical therapy and post-acute care utilization patterns and cost in total joint replacement. J Bone Joint Surg Am 2014;96:e165. [Crossref] [PubMed]
- Waterland JL, McCourt O, Edbrooke L, et al. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front Surg 2021;8:628848. [Crossref] [PubMed]
- Molenaar CJL, Papen-Botterhuis NE, Herrle F, et al. Prehabilitation, making patients fit for surgery - a new frontier in perioperative care. Innov Surg Sci 2019;4:132-8. [Crossref] [PubMed]
- Rombey T, Eckhardt H, Kiselev J, et al. Cost-effectiveness of prehabilitation prior to elective surgery: a systematic review of economic evaluations. BMC Med 2023;21:265. [Crossref] [PubMed]
- Bekelis K, Calnan D, Simmons N, et al. Effect of an Immersive Preoperative Virtual Reality Experience on Patient Reported Outcomes: A Randomized Controlled Trial. Ann Surg 2017;265:1068-73. [Crossref] [PubMed]
- Agarwal P, Mukerji G, Desveaux L, et al. Mobile App for Improved Self-Management of Type 2 Diabetes: Multicenter Pragmatic Randomized Controlled Trial. JMIR Mhealth Uhealth 2019;7:e10321. [Crossref] [PubMed]
- Bahado-Singh RO, Ibrahim A, Al-Wahab Z, et al. Precision gynecologic oncology: circulating cell free DNA epigenomic analysis, artificial intelligence and the accurate detection of ovarian cancer. Sci Rep 2022;12:18625. [Crossref] [PubMed]
- Meagher NS, Gorringe KL, Wakefield M, et al. Gene-Expression Profiling of Mucinous Ovarian Tumors and Comparison with Upper and Lower Gastrointestinal Tumors Identifies Markers Associated with Adverse Outcomes. Clin Cancer Res 2022;28:5383-95. [Crossref] [PubMed]
- DeVaux RS, Herschkowitz JI. Beyond DNA: the Role of Epigenetics in the Premalignant Progression of Breast Cancer. J Mammary Gland Biol Neoplasia 2018;23:223-35. [Crossref] [PubMed]
- Seth I, Bulloch G, Joseph K, et al. Use of Artificial Intelligence in the Advancement of Breast Surgery and Implications for Breast Reconstruction: A Narrative Review. J Clin Med 2023;12:5143. [Crossref] [PubMed]
- Qu M, Hou Y, Xu Y, et al. Precise positioning of an intraoral distractor using augmented reality in patients with hemifacial microsomia. J Craniomaxillofac Surg 2015;43:106-12. [Crossref] [PubMed]
- Müller M, Rassweiler MC, Klein J, et al. Mobile augmented reality for computer-assisted percutaneous nephrolithotomy. Int J Comput Assist Radiol Surg 2013;8:663-75. [Crossref] [PubMed]
- Hua J, Aziz S, Shum JW. Virtual Surgical Planning in Oral and Maxillofacial Surgery. Oral Maxillofac Surg Clin North Am 2019;31:519-30. [Crossref] [PubMed]
- Hammoudeh JA, Howell LK, Boutros S, et al. Current Status of Surgical Planning for Orthognathic Surgery: Traditional Methods versus 3D Surgical Planning. Plast Reconstr Surg Glob Open 2015;3:e307. [Crossref] [PubMed]
- Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med 2020;382:1679-81. [Crossref] [PubMed]
- Mullen-Fortino M, Rising KL, Duckworth J, et al. Presurgical Assessment Using Telemedicine Technology: Impact on Efficiency, Effectiveness, and Patient Experience of Care. Telemed J E Health 2019;25:137-42. [Crossref] [PubMed]
- Kamdar NV, Huverserian A, Jalilian L, et al. Development, Implementation, and Evaluation of a Telemedicine Preoperative Evaluation Initiative at a Major Academic Medical Center. Anesth Analg 2020;131:1647-56. [Crossref] [PubMed]
- Fitzpatrick K, Addie K, Shaw M, et al. Implementing an innovative, patient-centered approach to day case arthroplasty: improving patient outcomes through remote preoperative pharmacist consultations. Eur J Hosp Pharm 2023; Epub ahead of print. [Crossref] [PubMed]
- Afable MK, Gupte G, Simon SR, et al. Innovative Use Of Electronic Consultations In Preoperative Anesthesiology Evaluation At VA Medical Centers In New England. Health Aff (Millwood) 2018;37:275-82. [Crossref] [PubMed]
- Wright KD, Kim J, Ratcliffe CRD, et al. Pilot Examination of the Efficacy of the Internet-Delivered, Preoperative, Preparation Program (I-PPP). J Clin Psychol Med Settings 2021;28:627-36. [Crossref] [PubMed]
- Wu M, Tan H, Gao F, et al. Predicting the grade of hepatocellular carcinoma based on non-contrast-enhanced MRI radiomics signature. Eur Radiol 2019;29:2802-11. [Crossref] [PubMed]
- Yang DW, Jia XB, Xiao YJ, et al. Noninvasive Evaluation of the Pathologic Grade of Hepatocellular Carcinoma Using MCF-3DCNN: A Pilot Study. Biomed Res Int 2019;2019:9783106. [Crossref] [PubMed]
- Morshid A, Elsayes KM, Khalaf AM, et al. A machine learning model to predict hepatocellular carcinoma response to transcatheter arterial chemoembolization. Radiol Artif Intell 2019;1:e180021. [Crossref] [PubMed]
- Gross BC, Erkal JL, Lockwood SY, et al. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem 2014;86:3240-53. [Crossref] [PubMed]
- Martelli N, Serrano C, van den Brink H, et al. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 2016;159:1485-500. [Crossref] [PubMed]
- Valverde I, Gomez-Ciriza G, Hussain T, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardiothorac Surg 2017;52:1139-48. [Crossref] [PubMed]
- Tack P, Victor J, Gemmel P, et al. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online 2016;15:115. [Crossref] [PubMed]
- Olivieri LJ, Krieger A, Loke YH, et al. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Soc Echocardiogr 2015;28:392-7. [Crossref] [PubMed]
- Mittelstadt B. Ethics of the health-related internet of things: a narrative review. Ethics Inf Technol 2017;19:157-75. [Crossref]
- Roberts JS, Patterson AK, Uhlmann WR. Genetic testing for neurodegenerative diseases: Ethical and health communication challenges. Neurobiol Dis 2020;141:104871. [Crossref] [PubMed]
- Burton BN, Arastoo S, Wu S, et al. The Association of Medical Preoperative Evaluation Using Clinical Video Telehealth With Hospital Length of Stay: Descriptive Analysis. JMIR Form Res 2022;6:e38054. [Crossref] [PubMed]
- Riss P, Ralph G, Dwyer P. Open abdominal surgery: a diminishing art. Int Urogynecol J 2015;26:1557-8. [Crossref] [PubMed]
- Kim J, Chiesa N, Raazi M, et al. A systematic review of technology-based preoperative preparation interventions for child and parent anxiety. Can J Anaesth 2019;66:966-86. [Crossref] [PubMed]
Cite this article as: Vine M, Joseph K, Gibson D, Lim B, Chua M, Siu AHY, Dooreemeah D, Lee A, Cuomo R, Seth I. Innovative approaches to preoperative care including feasibility, efficacy, and ethical implications: a narrative review. AME Surg J 2024;4:1.


