
An unexpected complication of colonoscopy with acute bilateral lower limb ischemia successfully salvaged with early detection and emergency axillo-bifemoral bypass: a case report
Highlight box
Key finding
• Acute bilateral lower limb ischemia following colonoscopy: urgent computed tomography angiogram and vascular bypass salvage the limbs.
What is known and what is new?
• Bowel preparation can cause electrolyte imbalances and dehydration.
• Acute limb ischemia, as a sequela requiring urgent vascular intervention, is a rare complication, particularly in elderly patients with atherosclerotic risk factors.
What is the implication, and what should change now?
• Close monitoring, especially in elderly patients with atherosclerotic risk factors, is essential for early detection and management of thrombotic complications.
• Adequate hydration during bowel preparation and prolonged observation (at least 6 hours) following colonoscopy may help detect and manage potential complications like acute limb ischemia.
Introduction
Background
Colonoscopy is a routine procedure in general and gastrointestinal surgery services, as it is the gold standard for direct visualization of the entire colon to identify suspicious lesions (1). The peri-procedural preparation, including bowel preparation and sedation, often carries adverse effects that are less emphasized. Known complications of colonoscopy include vomiting, dehydration, abdominal pain, hypotension, syncopal episodes, heart rhythm disturbances, acute coronary syndrome, cerebral ischemia, and allergic reactions (2).
Rationale and knowledge gap
Although the majority of complications following colonoscopy are transient and self-limiting, more severe and uncommon complications can occur. Among these, acute limb ischemia is a rare and potentially life-threatening event that has not been widely reported in association with colonoscopy. The pathophysiology behind such complications is not well understood, and few studies have examined the mechanisms that might link colonoscopy to subsequent vascular events. There is also limited discussion in the literature regarding the increased vulnerability of elderly patients with atherosclerotic risk factors who may face an elevated risk of severe complications post-colonoscopy.
Objective
Here, we report the case of a 73-year-old woman who developed acute bilateral lower limb ischemia 6 hours after colonoscopy, which was successfully salvaged through emergency vascular bypass surgery. We discuss the potential etiopathogenesis of this acute limb ischemia in the context of colonoscopy and emphasize the importance of careful peri-procedural management in elderly patients with atherosclerotic risk factors undergoing the procedure. The sequelae of acute lower limb ischemia following colonoscopy are rare, and reporting this case provides a unique clinical contribution. We present this case in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-24-44/rc).
Case presentation
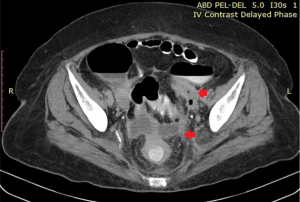
A 73-year-old woman presented with generalized cramping abdominal pain and abdominal bloating for 1 week. She had hypertension and dyslipidemia on simvastatin 20 mg once at night (ON), amlodipine 10 mg once daily (OD), losartan 50 mg OD and atenolol 50 mg OD but was a non-smoker. Her initial computed tomography (CT) scan of the abdomen and pelvis revealed suspected sigmoid diverticular disease with a multiloculated, thick-walled collection and air pockets extending from the bilateral retroperitoneal region into the pouch of Douglas (Figure 1). There was also mural thickening and narrowing of the sigmoid colon. She was treated with antibiotics [2 weeks of intravenous (IV) cefoperazone 1 g twice a day (BD) and IV metronidazole for 2 weeks and another 2 weeks of oral cefuroxime 500 mg BD], and a follow-up CT scan after 1 month showed a reduction in the size of the collection.
She was scheduled for an elective colonoscopy 2 months later. On the day before the procedure, she underwent bowel preparation with polyethylene glycol, administered at 6 pm and 8 pm, and at 6 am on the day of the procedure. Colonoscopy was performed at noon and revealed a single diverticulum at the distal sigmoid colon. The procedure was limited by a tight angulation of the colon that prevented further advancement of the endoscope. During the procedure, she received 2 mg of midazolam and 50 mcg of fentanyl.
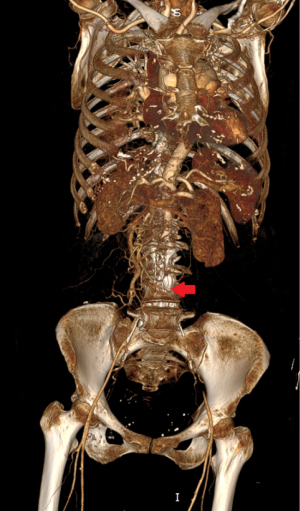
Six hours after the procedure, the patient developed severe pain, paresthesia, and paresis in both lower limbs. The event occurred after she walked to the bathroom; she did not experience any trauma or fall. Clinically, both legs were cold up to the thighs, and there were no palpable pulses in the infrainguinal region. Bedside Doppler ultrasound revealed a calcified infrarenal aorta with no color flow observed. The common and external iliac arteries were obscured by bowel shadow. An urgent CT angiogram of the bilateral lower limbs revealed long-segment thrombosis of the distal infrarenal abdominal aorta at the level of L2, extending to the bilateral common iliac arteries and common femoral arteries (Figure 2). She was diagnosed with bilateral acute-on-chronic lower limb ischemia secondary to distal aortic occlusion (Rutherford IIA). She was started on a heparin drip, and both the chest X-ray and echocardiography were unremarkable.
The patient underwent bilateral femoral embolectomy, right common femoral artery endarterectomy, and left axillo-bifemoral bypass grafting (Figure 3). Postoperatively, she developed a hematoma at the axillo-bifemoral anastomosis site, which required a left axilla wound exploration, evacuation of the hematoma, and hemostasis on postoperative day 4. She was discharged 15 days after surgery with no further pain in her lower limbs and was able to ambulate with minimal assistance. Postoperative medications included T. Cardiprin 100 mg once daily and T. Atorvastatin 40 mg once nightly. At the 3-month follow-up, she reported no recurrence of symptoms in either the abdomen or lower limbs.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained for the publication of this case report and accompanying images from the patient. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
This case highlights a rare and severe complication following colonoscopy—acute bilateral lower limb ischemia. The patient, a 73-year-old woman with pre-existing hypertension and dyslipidemia, developed this condition 6 hours after the procedure, which was successfully managed with emergency vascular bypass surgery. Our findings suggest that dehydration and electrolyte disturbances from bowel preparation, combined with the patient’s pre-existing atherosclerotic risk factors (3,4), may have contributed to the development of acute-on-chronic limb ischemia. The early detection and prompt surgical intervention were key to salvaging the limb.
Strengths and limitations
The primary strength of this case report lies in its presentation of a rare and serious complication of colonoscopy, adding valuable insight into the potential mechanisms of acute limb ischemia in the context of a routine procedure. The report also emphasizes the importance of peri-procedural monitoring, particularly in elderly patients with known cardiovascular risk factors. However, as a single case report, the findings are limited in terms of generalizability. The underlying mechanisms of acute limb ischemia in this context remain speculative and require further validation through larger studies.
Comparison with similar research
While complications following colonoscopy are well-documented, particularly gastrointestinal and cardiorespiratory issues, the occurrence of acute limb ischemia is exceptionally rare. Existing literature focuses more on common complications such as hypotension, abdominal pain, and minor arrhythmias (5). A retrospective study of 200,000 patients undergoing colonoscopy found that cardiorespiratory complications occurred in only 0.06% of cases, with age identified as a significant risk factor (6). The connection between dehydration, electrolyte imbalances, and acute limb ischemia has not been extensively explored, and this case contributes new evidence to that limited body of research.
Explanations of findings
Several factors likely contributed to the development of acute limb ischemia in this patient. Atherosclerosis, influenced by the patient’s age and comorbidities, predisposes the arteries to thrombosis and reduces the blood flow to peripheral limbs. Dehydration, a common complication of bowel preparation, likely exacerbated this risk by increasing blood viscosity and promoting clot formation (7,8). Electrolyte imbalances, particularly magnesium deficiency, are known to contribute to both atherosclerosis and thrombogenesis (9,10). These factors, combined with the stress of the colonoscopy procedure itself, likely led to the development of acute-on-chronic limb ischemia. In terms of sedation, midazolam combined with fentanyl is commonly used, but there are no reports in the literature linking these sedative agents with the exacerbation of acute limb ischemia (11).
Implications and actions needed
The findings from this case underscore the importance of proper peri-procedural management in elderly patients undergoing colonoscopy, especially those with known risk factors for cardiovascular and thrombotic events. We recommend ensuring adequate hydration during bowel preparation, particularly in older patients, and closely monitoring electrolyte levels. Additionally, these patients may benefit from extended observation periods (at least 6 hours post-procedure) to identify and address any potential thrombotic events early. Further prospective studies are necessary to develop targeted guidelines for peri-procedural care in elderly individuals, especially those with cardiovascular comorbidities, to mitigate the risk of serious complications such as acute limb ischemia.
Conclusions
Patients with a high risk of atherosclerosis and thrombosis should be adequately hydrated before, during, and after colonoscopy. In high-risk cases, prolonged observation following the procedure may help prevent missed thrombotic events that could lead to limb loss. Further research into peri-procedural management for these patients is warranted to optimize outcomes.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-24-44/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-24-44/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-24-44/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained for the publication of this case report and accompanying images from the patient. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ASGE Standards of Practice Committee. Bowel preparation before colonoscopy. Gastrointest Endosc 2015;81:781-94. [Crossref] [PubMed]
- Latos W, Aebisher D, Latos M, et al. Colonoscopy: Preparation and Potential Complications. Diagnostics (Basel) 2022;12:747. [Crossref] [PubMed]
- Wang JC, Bennett M. Aging and atherosclerosis: mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ Res 2012;111:245-59. [Crossref] [PubMed]
- Luca AC, David SG, David AG, et al. Atherosclerosis from Newborn to Adult-Epidemiology, Pathological Aspects, and Risk Factors. Life (Basel) 2023;13:2056. [Crossref] [PubMed]
- Reumkens A, van der Zander Q, Winkens B, et al. Electrolyte disturbances after bowel preparation for colonoscopy: Systematic review and meta-analysis. Dig Endosc 2022;34:913-26. [Crossref] [PubMed]
- Piechocki M, Przewłocki T, Pieniążek P, et al. A Non-Coronary, Peripheral Arterial Atherosclerotic Disease (Carotid, Renal, Lower Limb) in Elderly Patients-A Review: Part I-Epidemiology, Risk Factors, and Atherosclerosis-Related Diversities in Elderly Patients. J Clin Med 2024;13:1471. [Crossref] [PubMed]
- Lichtenstein GR, Cohen LB, Uribarri J. Review article: Bowel preparation for colonoscopy--the importance of adequate hydration. Aliment Pharmacol Ther 2007;26:633-41. [Crossref] [PubMed]
- Holte K, Nielsen KG, Madsen JL, et al. Physiologic effects of bowel preparation. Dis Colon Rectum 2004;47:1397-402. [Crossref] [PubMed]
- Maier JA, Malpuech-Brugère C, Zimowska W, et al. Low magnesium promotes endothelial cell dysfunction: implications for atherosclerosis, inflammation and thrombosis. Biochim Biophys Acta 2004;1689:13-21. [Crossref] [PubMed]
- Baskurt OK, Meiselman HJ. Iatrogenic hyperviscosity and thrombosis. Semin Thromb Hemost 2012;38:854-64. [Crossref] [PubMed]
- Childers RE, Williams JL, Sonnenberg A. Practice patterns of sedation for colonoscopy. Gastrointest Endosc 2015;82:503-11. [Crossref] [PubMed]
Cite this article as: Chin WY, Tan JH, Othman ZB, Pillay KK. An unexpected complication of colonoscopy with acute bilateral lower limb ischemia successfully salvaged with early detection and emergency axillo-bifemoral bypass: a case report. AME Surg J 2024;4:25.



